Our objective is to share our experience in neurogenic tumors of the sacral area, an uncommon disease, and assess approaches, intraoperative techniques, complications and clinical course of patients in a case series.
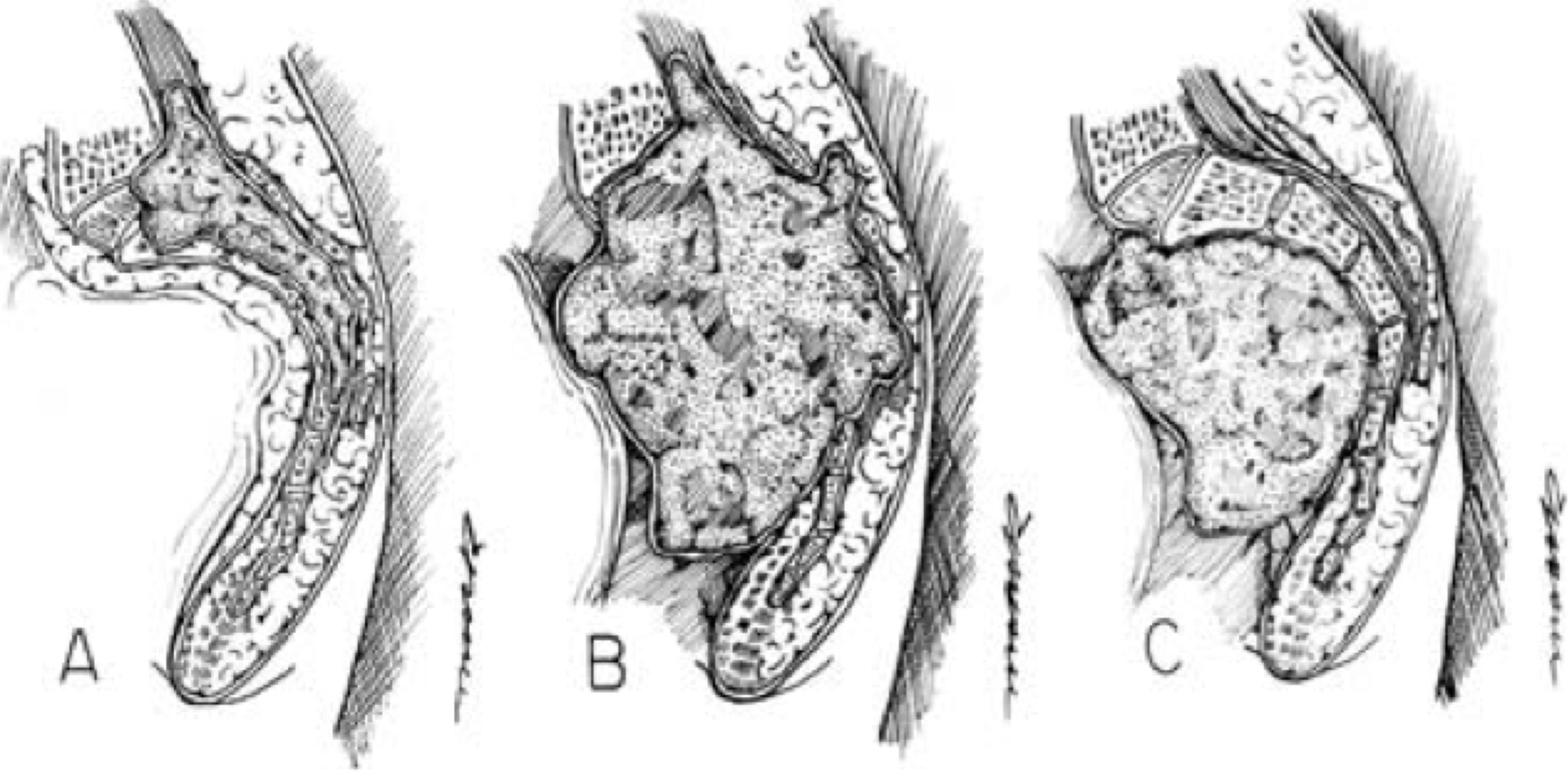
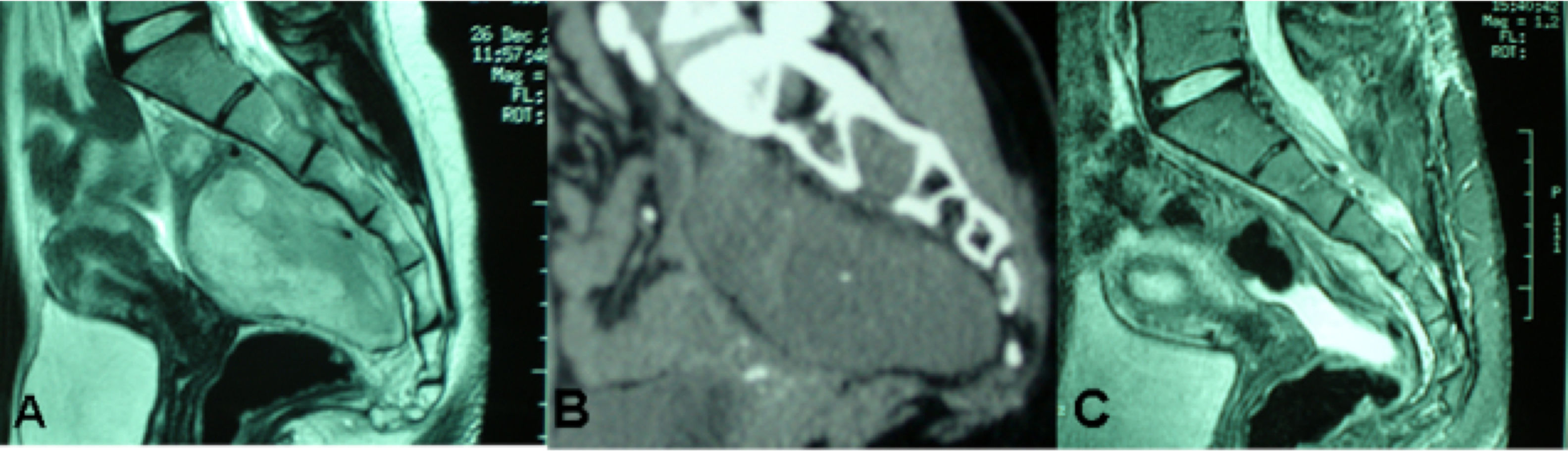
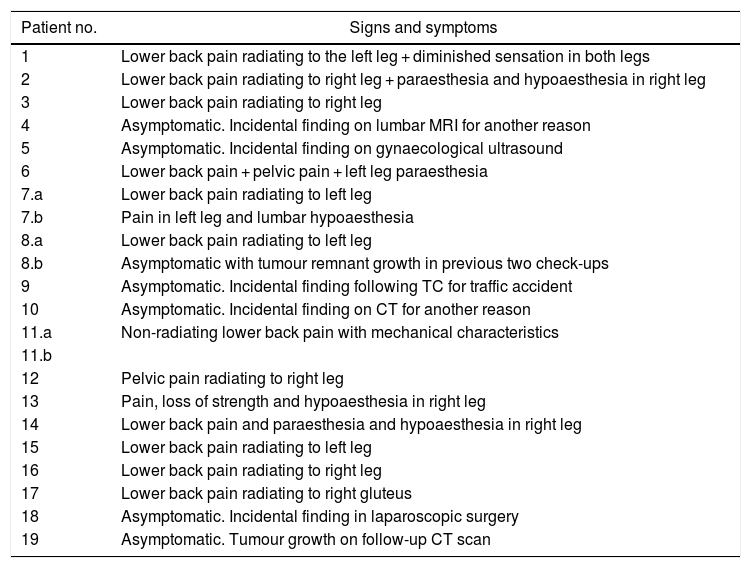
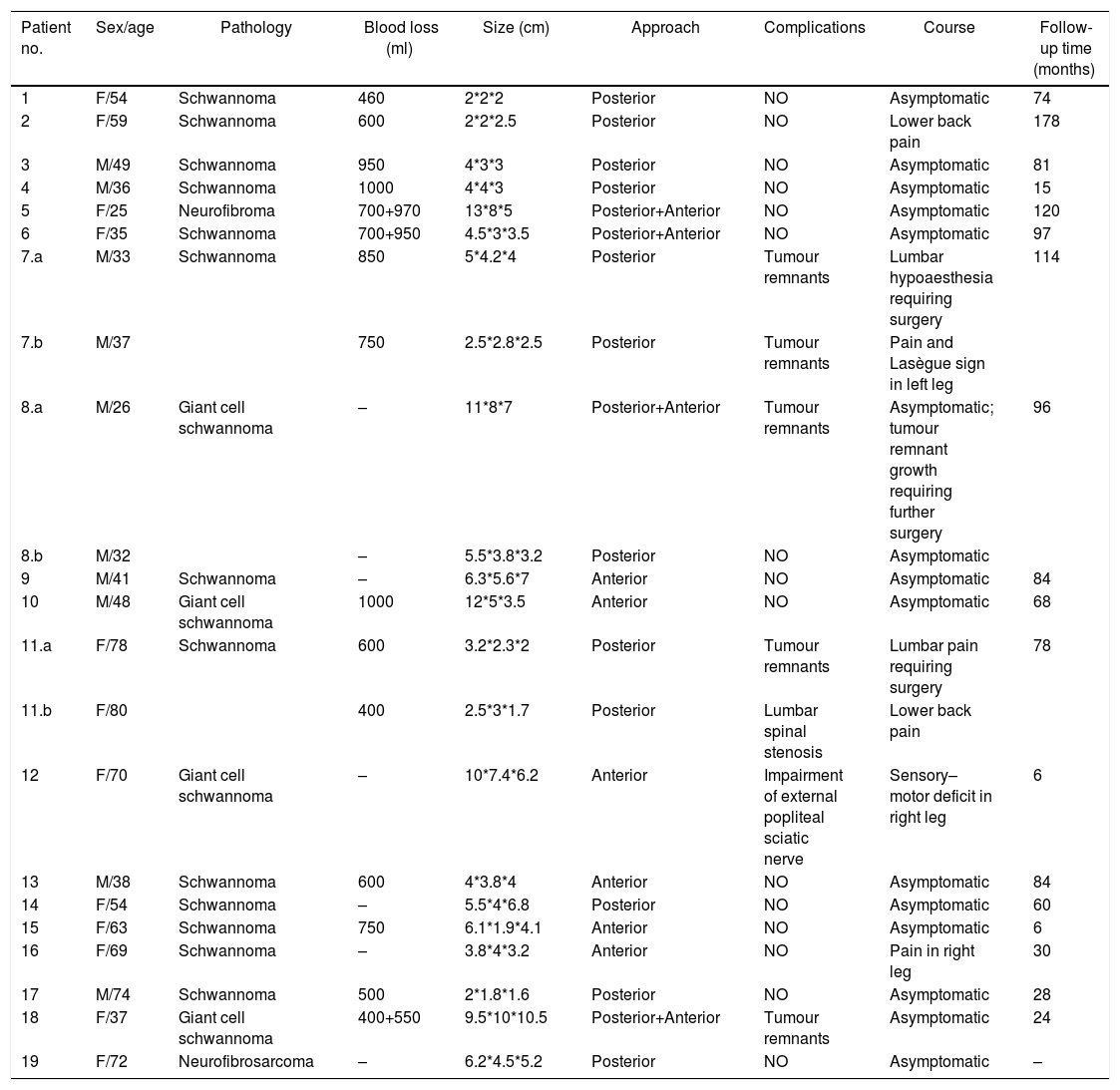
MethodsWe conducted a retrospective analysis of 19 cases of patients with neurogenic tumors in the sacral area who were diagnosed and underwent surgery at our center. Of them, 8 were male and 11 were female. They had a mean age at diagnosis of 51 years (with an age range of 25–78 years). Six patients were asymptomatic and were diagnosed incidentally, while the majority (11 patients) presented with lumbar pain accompanied by other symptoms: pain radiating to the legs, pelvic pain, sensory alterations and loss of strength in the legs. Two patients presented with another primary symptom on diagnosis: pain in the pelvic region and in the left leg. All patients underwent a least one imaging test (MRI/CT scan). Nine patients had tumors limited to the sacrum or with subsequent spread, with surgery via the posterior route. In 6 cases, an exclusively anterior approach was employed owing to the pre-sacral location of the tumor; 4 cases required both an anterior and posterior approach.
ResultsThe 6 patients who were asymptomatic at diagnosis continued to have no symptoms after surgery. In 8 patients, symptoms resolved after surgery, and at discharge 4 had pain in the lumbar region or legs, which improved in subsequent consultations. One patient had symptoms consistent with motor and sensory deficit in the right leg deriving from impairment of the external popliteal sciatic nerve. The mean follow-up period was 69 months (6–178 months). Histologically, 17 cases were classified as schwannomas, one case was classified as neurofibroma, and one case was classified as neurofibrosarcoma, which received radiotherapy. Three patients with benign histologies had further surgery for local recurrences.
ConclusionsWhen selecting the approach, the large size that these tumors can reach, their relationship with structures, and their anterior or posterior spread should be taken in to account. Resecting the tumor mass as much as possible provides greater benefit to the patient, as this decreases the odds of tumor recurrence without increasing intraoperative and postoperative complications when multidisciplinary teams are also used.
Nuestro objetivo es compartir nuestra experiencia en tumores neurogénicos del área sacra, una patología infrecuente, valorando las vías de abordaje, técnicas intraoperatorias, complicaciones y evolución de los pacientes en una serie de casos.
MétodosRealizamos un análisis retrospectivo de 19 casos de tumores neurogénicos de la región sacra diagnosticados y operados en nuestro centro, de los cuáles 8 eran varones y 11 mujeres, registrando una edad media al diagnóstico de 51 años (con un rango de edades entre 25 y 78 años). Seis se encontraban asintomáticos y fueron diagnosticados incidentalmente, mientras que la mayoría (11 pacientes) presentaban dolor lumbar acompañado de otros síntomas: dolor irradiado a miembros inferiores (MMII), dolor pélvico, alteraciones sensitivas y pérdida de fuerza en MMII. Dos pacientes presentaban otro síntoma principal al diagnóstico: dolor pélvico y en miembro inferior izquierdo (MII). A todos los pacientes se les realizó como mínimo una prueba de imagen (RM/TC). 9 pacientes tenían tumores limitados al sacro o con extensión posterior, practicándose una intervención por vía posterior. En 6 se realizó un abordaje exclusivamente por vía anterior debido a la localización presacra de la tumoración; y en 4 de ellos fue preciso un abordaje tanto anterior como posterior.
ResultadosLos 6 pacientes asintomáticos al diagnóstico continuaron sin síntomas tras la intervención. En 8 desaparecieron los síntomas después de la cirugía, y al alta 4 presentaron dolor lumbar o de miembros que mejoró en consultas sucesivas. Una paciente presentó clínica consistente en déficit motor y sensitivo en el miembro inferior derecho derivada de la afectación del nervio ciático poplíteo externo. El tiempo medio de seguimiento fue de 69 meses (desde 6 hasta 178 meses). Histológicamente 17 casos se catalogaron como Schwannomas, un caso neurofibroma y un neurofibrosarcoma, que recibió radioterapia. Tres pacientes con histología benigna fueron reintervenidos por recidivas locales.
ConclusionesSe debe considerar el gran tamaño que pueden alcanzar estos tumores, su relación con estructuras y la extensión anterior o posterior para seleccionar el abordaje. Resecar la mayor cantidad posible de masa tumoral aporta un mayor beneficio al paciente; al disminuir las posibilidades de recidiva tumoral sin aumentar las complicaciones intra y postoperatorias cuando se utilizan además equipos multidisciplinares.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.