O-FUN-30 - Thalamic deep brain stimulation for neuropathic pain: efficacy at 3 years follow-up
1Departamento de Neurocirugia, Hospital de São João and Faculdade da Medicina, Universidade do Porto. 2Center for Neurosciences CUF Porto. 3Department of Neurosurgery and Nuffield Department of Surgery, Oxford University Hospitals, Oxford.
Objectives: Chronic neuropathic pain is estimated to affect 3-4,5% of the worldwide population, being a seriously burden to society. Deep Brain Stimulation (DBS) is already established for movement disorders and also used to treat some “off-label” conditions. However, for the treatment of neuropathic pain has shown variable outcomes and few studies were performed in the last decade. This study prospectively evaluated the efficacy at 3 years of DBS for neuropathic pain.
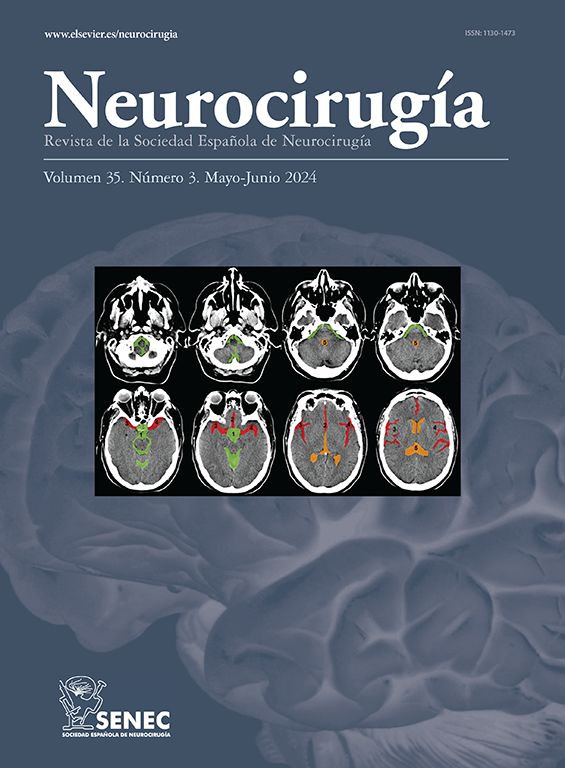
Material and methods: Twelve patients were submitted to a 36 months follow-up in a single-center case series. Five had phantom limb pain after amputation and seven deafferentation pain after brachial plexus avulsion (BPA), all from traumas. To evaluate the efficacy of DBS, patient-reported outcome measures were collated before and after surgery, using a visual analog scale (VAS) score, 36-Item Short-Form Health Survey (SF-36), Brief Pain Inventory (BPI), and University of Washington Neuropathic Pain Score (UWNPS).
Results: Contralateral, ventroposterolateral sensory thalamic DBS was performed in twelve patients with chronic neuropathic pain over 29 months. A postoperative trial of externalized DBS failed in one patient with BPA. Eleven patients proceeded to implantation and gained improvement in pain scores at 36 months, with the exception of one patient with phantom limb pain after amputation that was not followed-up after 12 months. Mean DBS parameters were 2.5 V, 213 microseconds, and 25 Hz. No surgical complications or stimulation side effects were noted. After 36 months, mean pain relief was sustained in the overall group: VAS score was improved from before surgery by 60.4% ± 30.4% (p = 0.001), SF-36 improved by 33.9% ± 79.9% (p = 1.000), UWNPS improved by 39.7% ± 43.5% (p = 0.073) and BPI improved by 52.2% ± 37.4% (p = 0.05).
Conclusions: DBS demonstrated efficacy at 3 years for chronic neuropathic pain after traumatic amputation and BPA, being the amputation subgroup the one that improved more, with benefits sustained across all pain outcome measures.