Carotid cross-clamping during carotid endarterectomy might lead to intraoperative neurologic deficits, increasing stroke/death risk. If deficits are detected, carotid shunting has been recommended to reduce the risk of stroke. However, shunting may sustain a specific chance of embolic events and subsequently incurring harm. Current evidence is still questionable regarding its clear benefit. The aim is to determine whether a policy of selective shunt impacts the complication rate following an endarterectomy.
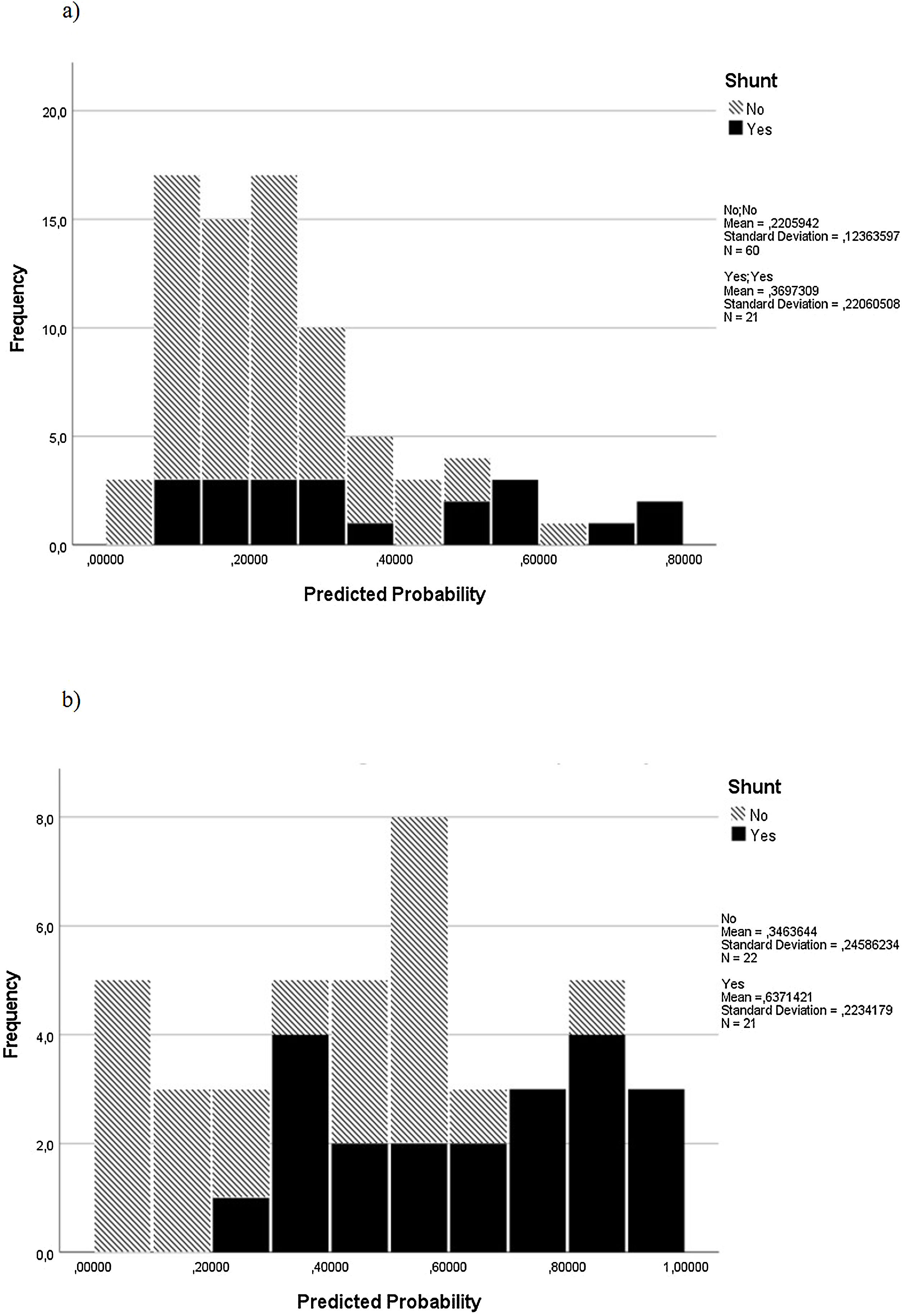
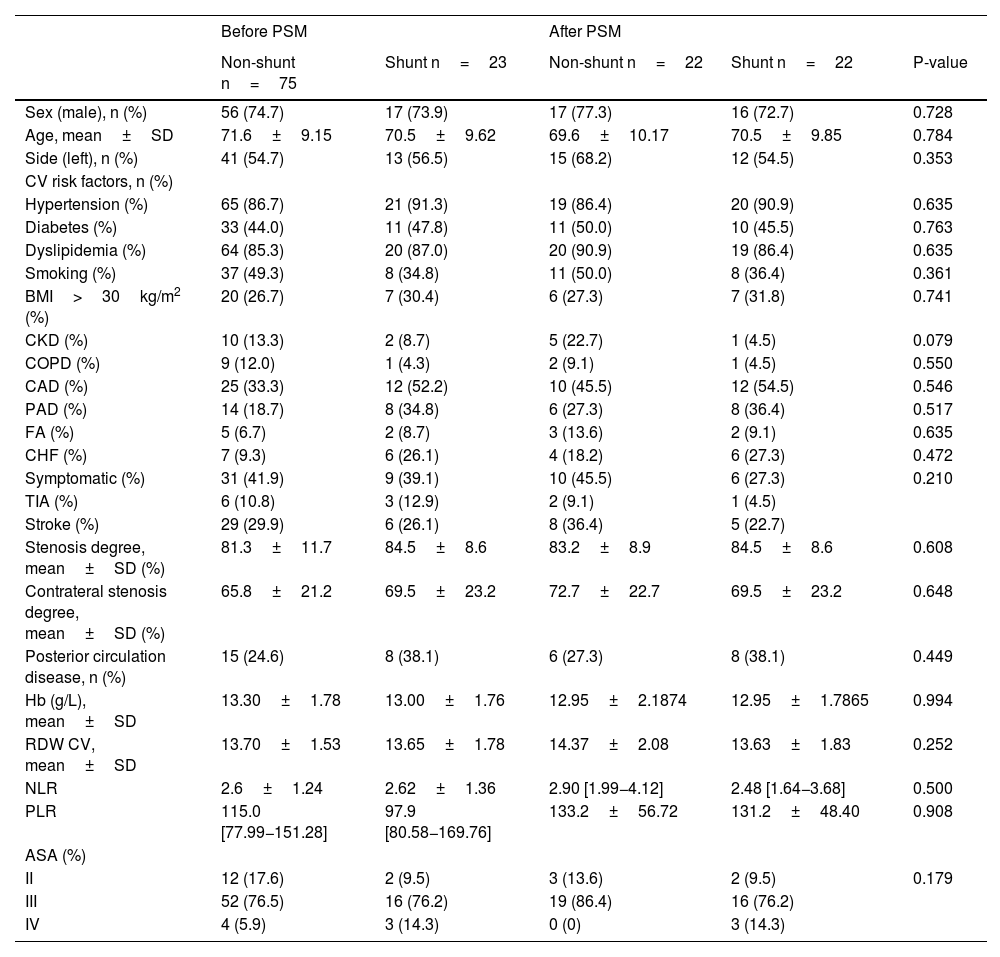
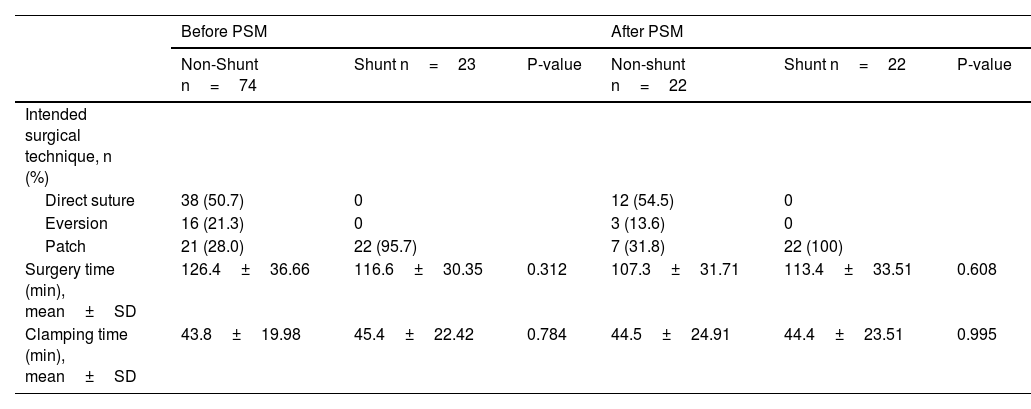
Material and methodsFrom January 2013 to May 2021, all patients undergoing carotid endarterectomy under regional anesthesia with intraoperative neurologic alteration were retrieved. Patients submitted to selective shunt were compared to a non-shunt group. A 1:1 propensity score matching (PSM) was performed. Differences between the groups and clinical outcomes were calculated, resorting to univariate analysis.
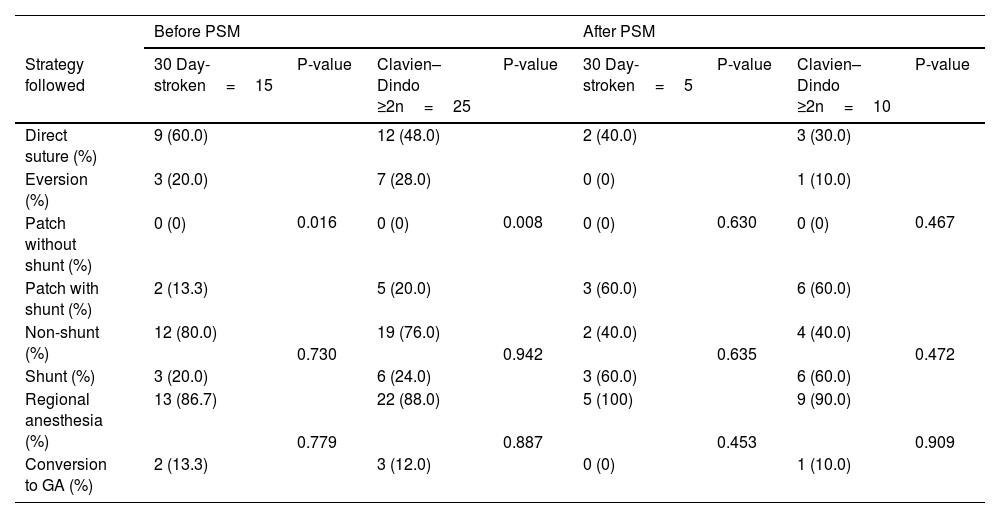
ResultsNinety-eight patients were selected, from which 23 were operated on using a shunt. After PSM, 22 non-shunt patients were compared to 22 matched shunted patients. Concerning demographics and comorbidities, both groups were comparable to pre and post-PSM, except for chronic heart failure, which was more prevalent in shunted patients (26.1%, P=0.036) in pre-PSM analysis. Regarding 30-day stroke and score Clavien–Dindo ≥2, no significant association was found (P=0.730, P=0.635 and P=0.942, P=0.472, correspondingly, for pre and post-PSM).
ConclusionsIn this cohort, resorting to shunting did not demonstrate an advantage regarding 30-day stroke or a Clavien–Dindo ≥ 2 rates. Nevertheless, additional more extensive studies are mandatory to achieve precise results concerning the accurate utility of carotid shunting in this subset of patients under regional anesthesia.
El pinzamiento carotídeo durante la endarterectomía carotídea podría provocar déficits neurológicos intraoperatorios, lo que aumenta el riesgo de accidente cerebrovascular/muerte. Si se detectan déficits, se ha recomendado la derivación carotídea para reducir el riesgo de accidente cerebrovascular. Sin embargo, la derivación puede sostener una posibilidad específica de eventos embólicos y, posteriormente, provocar daños. La evidencia actual aún es cuestionable con respecto a su claro beneficio. El objetivo es determinar si una política de derivación selectiva afecta la tasa de complicaciones después de una endarterectomía.
Material y métodosDesde enero de 2013 hasta mayo de 2021 se recuperaron todos los pacientes sometidos a endarterectomía carotídea bajo anestesia regional con alteración neurológica intraoperatoria. Los pacientes sometidos a derivación selectiva se compararon con un grupo sin derivación. Se realizó una coincidencia de puntuación de propensión (PSM) 1:1. Se calcularon las diferencias entre los grupos y los resultados clínicos recurriendo al análisis univariado.
ResultadosSe seleccionaron 98 pacientes, de los cuales 23 fueron intervenidos mediante derivación. Después de la PSM, se compararon 22 pacientes sin derivación con 22 pacientes emparejados con derivación. Con respecto a la demografía y las comorbilidades, ambos grupos fueron comparables a los de antes y después de la PSM, excepto por la insuficiencia cardíaca crónica, que fue más prevalente en los pacientes con derivación (26,1 %, P=0,036) en el análisis previo a la PSM. En cuanto al accidente cerebrovascular a los 30 días y la puntuación de Clavien–Dindo ≥2, no se encontró asociación significativa (P=0,730, P=0,635 y P=0,942, P=0,472, correspondientemente, para pre y post-PSM).
ConclusionesEn esta cohorte, recurrir a la derivación no demostró una ventaja con respecto a las tasas de ictus a los 30 días o Clavien–Dindo ≥ 2. Sin embargo, se requieren estudios adicionales más extensos para lograr resultados precisos sobre la utilidad precisa de la derivación carotídea en este subgrupo de pacientes bajo anestesia regional.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.