Compartir
array:23 [
"pii" => "S1130147322000586"
"issn" => "11301473"
"doi" => "10.1016/j.neucir.2022.04.003"
"estado" => "S300"
"fechaPublicacion" => "2023-03-01"
"aid" => "553"
"copyright" => "Sociedad Española de Neurocirugía"
"copyrightAnyo" => "2022"
"documento" => "simple-article"
"crossmark" => 1
"subdocumento" => "crp"
"cita" => "Neurocirugia. 2023;34:97-100"
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"itemSiguiente" => array:19 [
"pii" => "S1130147322000598"
"issn" => "11301473"
"doi" => "10.1016/j.neucir.2022.05.001"
"estado" => "S300"
"fechaPublicacion" => "2023-03-01"
"aid" => "554"
"copyright" => "Sociedad Española de Neurocirugía"
"documento" => "simple-article"
"crossmark" => 1
"subdocumento" => "crp"
"cita" => "Neurocirugia. 2023;34:101-4"
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"en" => array:13 [
"idiomaDefecto" => true
"cabecera" => "<span class="elsevierStyleTextfn">Case Report</span>"
"titulo" => "Symptomatic sacral Tarlov cyst: Case report and review of literature"
"tienePdf" => "en"
"tieneTextoCompleto" => "en"
"tieneResumen" => array:2 [
0 => "en"
1 => "es"
]
"paginas" => array:1 [
0 => array:2 [
"paginaInicial" => "101"
"paginaFinal" => "104"
]
]
"titulosAlternativos" => array:1 [
"es" => array:1 [
"titulo" => "Quiste de Tarlov sacro sintomatico: presentacion de un caso y revision de la literatura"
]
]
"contieneResumen" => array:2 [
"en" => true
"es" => true
]
"contieneTextoCompleto" => array:1 [
"en" => true
]
"contienePdf" => array:1 [
"en" => true
]
"resumenGrafico" => array:2 [
"original" => 0
"multimedia" => array:7 [
"identificador" => "fig0005"
"etiqueta" => "Fig. 1"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr1.jpeg"
"Alto" => 674
"Ancho" => 1340
"Tamanyo" => 110293
]
]
"descripcion" => array:1 [
"en" => "<p id="spar0015" class="elsevierStyleSimplePara elsevierViewall">Preoperative MRI. (A) Sagital view showing a sacral Tarlov cyst. (B) Axial view where it is possible to identify the nerve roots in the anterior wall of the cyst (arrows).</p>"
]
]
]
"autores" => array:1 [
0 => array:2 [
"autoresLista" => "Angel Horcajadas Almansa, Ana M. Jorques Infante, Ana M. Román Cutillas, Luis Guzmán Álvarez"
"autores" => array:4 [
0 => array:2 [
"nombre" => "Angel Horcajadas"
"apellidos" => "Almansa"
]
1 => array:2 [
"nombre" => "Ana M. Jorques"
"apellidos" => "Infante"
]
2 => array:2 [
"nombre" => "Ana M. Román"
"apellidos" => "Cutillas"
]
3 => array:2 [
"nombre" => "Luis Guzmán"
"apellidos" => "Álvarez"
]
]
]
]
]
"idiomaDefecto" => "en"
"Traduccion" => array:1 [
"en" => array:9 [
"pii" => "S252984962200096X"
"doi" => "10.1016/j.neucie.2022.11.021"
"estado" => "S300"
"subdocumento" => ""
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"idiomaDefecto" => "en"
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S252984962200096X?idApp=UINPBA00004B"
]
]
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S1130147322000598?idApp=UINPBA00004B"
"url" => "/11301473/0000003400000002/v1_202303021130/S1130147322000598/v1_202303021130/en/main.assets"
]
"itemAnterior" => array:19 [
"pii" => "S1130147322000422"
"issn" => "11301473"
"doi" => "10.1016/j.neucir.2022.03.003"
"estado" => "S300"
"fechaPublicacion" => "2023-03-01"
"aid" => "548"
"copyright" => "Sociedad Española de Neurocirugía"
"documento" => "simple-article"
"crossmark" => 1
"subdocumento" => "crp"
"cita" => "Neurocirugia. 2023;34:93-6"
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"en" => array:13 [
"idiomaDefecto" => true
"cabecera" => "<span class="elsevierStyleTextfn">Case report</span>"
"titulo" => "Sphenoidal meningoencephalocele associated with CSF fistula and arteriovenous malformation Spetzler-Martin V: A case report"
"tienePdf" => "en"
"tieneTextoCompleto" => "en"
"tieneResumen" => array:2 [
0 => "en"
1 => "es"
]
"paginas" => array:1 [
0 => array:2 [
"paginaInicial" => "93"
"paginaFinal" => "96"
]
]
"titulosAlternativos" => array:1 [
"es" => array:1 [
"titulo" => "Meningoencefalocele esfenoidal asociado a fístula de líquido cefalorraquídeo y malformación arteriovenosa Spetzler-Martin V: reporte de caso"
]
]
"contieneResumen" => array:2 [
"en" => true
"es" => true
]
"contieneTextoCompleto" => array:1 [
"en" => true
]
"contienePdf" => array:1 [
"en" => true
]
"resumenGrafico" => array:2 [
"original" => 0
"multimedia" => array:7 [
"identificador" => "fig0010"
"etiqueta" => "Fig. 2"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr2.jpeg"
"Alto" => 1361
"Ancho" => 1508
"Tamanyo" => 150819
]
]
"descripcion" => array:1 [
"en" => "<p id="spar0040" class="elsevierStyleSimplePara elsevierViewall">Panel a. Brain T2-weighted MRI Axial view, showing the meningoencephalocele through the right greater sphenoid wing. Panel b. Frontal projection with, arterial, capillary and venous phase. Arterial phase shows a diffuse AVM nidus with main supply from multiple branches of the middle cerebral artery and venous phase, with partial drainage in the deep venous system through the right basal vein of Rosenthal.</p>"
]
]
]
"autores" => array:1 [
0 => array:2 [
"autoresLista" => "Esteban Ramírez-Ferrer, Rafael Aponte-Caballero, Maria Paula Aguilera-Pena, Santiago David Mendoza-Ayús, Luis Alejandro Osorio-Bohorquez, William Mauricio Riveros-Castillo"
"autores" => array:6 [
0 => array:2 [
"nombre" => "Esteban"
"apellidos" => "Ramírez-Ferrer"
]
1 => array:2 [
"nombre" => "Rafael"
"apellidos" => "Aponte-Caballero"
]
2 => array:2 [
"nombre" => "Maria Paula"
"apellidos" => "Aguilera-Pena"
]
3 => array:2 [
"nombre" => "Santiago David"
"apellidos" => "Mendoza-Ayús"
]
4 => array:2 [
"nombre" => "Luis Alejandro"
"apellidos" => "Osorio-Bohorquez"
]
5 => array:2 [
"nombre" => "William Mauricio"
"apellidos" => "Riveros-Castillo"
]
]
]
]
]
"idiomaDefecto" => "en"
"Traduccion" => array:1 [
"en" => array:9 [
"pii" => "S2529849622000922"
"doi" => "10.1016/j.neucie.2022.11.017"
"estado" => "S300"
"subdocumento" => ""
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"idiomaDefecto" => "en"
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2529849622000922?idApp=UINPBA00004B"
]
]
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S1130147322000422?idApp=UINPBA00004B"
"url" => "/11301473/0000003400000002/v1_202303021130/S1130147322000422/v1_202303021130/en/main.assets"
]
"en" => array:20 [
"idiomaDefecto" => true
"cabecera" => "<span class="elsevierStyleTextfn">Case Report</span>"
"titulo" => "Covered stent delivery in tortuous internal carotid artery for treatment of direct carotid cavernous fistula"
"tieneTextoCompleto" => true
"paginas" => array:1 [
0 => array:2 [
"paginaInicial" => "97"
"paginaFinal" => "100"
]
]
"autores" => array:1 [
0 => array:4 [
"autoresLista" => "Mehrnoush Gorjian, Scott Raymond, Matthew Koch, Aman Patel"
"autores" => array:4 [
0 => array:4 [
"nombre" => "Mehrnoush"
"apellidos" => "Gorjian"
"email" => array:1 [
0 => "mgorjian@salud.unm.edu"
]
"referencia" => array:2 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">a</span>"
"identificador" => "aff0005"
]
1 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">*</span>"
"identificador" => "cor0005"
]
]
]
1 => array:3 [
"nombre" => "Scott"
"apellidos" => "Raymond"
"referencia" => array:1 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">b</span>"
"identificador" => "aff0010"
]
]
]
2 => array:3 [
"nombre" => "Matthew"
"apellidos" => "Koch"
"referencia" => array:1 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">c</span>"
"identificador" => "aff0015"
]
]
]
3 => array:3 [
"nombre" => "Aman"
"apellidos" => "Patel"
"referencia" => array:1 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">d</span>"
"identificador" => "aff0020"
]
]
]
]
"afiliaciones" => array:4 [
0 => array:3 [
"entidad" => "Department of Neurology, University of New Mexico, 900 Camino de Salud, Albuquerque, NM 87131, United States"
"etiqueta" => "a"
"identificador" => "aff0005"
]
1 => array:3 [
"entidad" => "Department of Radiology, University of Vermont Medical Center, 111 Colchester Ave, Burlington, VT 05401, United States"
"etiqueta" => "b"
"identificador" => "aff0010"
]
2 => array:3 [
"entidad" => "Department of Neurosurgery, University of Florida, 1505 SW archer Rd, Gainesville, FL 32608, United States"
"etiqueta" => "c"
"identificador" => "aff0015"
]
3 => array:3 [
"entidad" => "Department of Neurosurgery, Massachusetts General Hospital, 55 Fruit St, Boston, MA 02114, United States"
"etiqueta" => "d"
"identificador" => "aff0020"
]
]
"correspondencia" => array:1 [
0 => array:3 [
"identificador" => "cor0005"
"etiqueta" => "⁎"
"correspondencia" => "<span class="elsevierStyleItalic">Corresponding author</span>."
]
]
]
]
"titulosAlternativos" => array:1 [
"es" => array:1 [
"titulo" => "Colocación de un stent cubierto en una arteria carótida interna tortuosa para el tratamiento de la fístula carótida cavernosa directa"
]
]
"resumenGrafico" => array:2 [
"original" => 0
"multimedia" => array:7 [
"identificador" => "fig0015"
"etiqueta" => "Fig. 3"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr3.jpeg"
"Alto" => 773
"Ancho" => 1607
"Tamanyo" => 177474
]
]
"descripcion" => array:1 [
"en" => "<p id="spar0025" class="elsevierStyleSimplePara elsevierViewall">Follow up DSA AP (A) and lateral (B) views 3 months postoperatively shows no residual dCCF of the left cavernous ICA and no residual filling of the left ophthalmic artery pseudoaneurysm.</p>"
]
]
]
"textoCompleto" => "<span class="elsevierStyleSections"><span id="sec0005" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0025">Introduction</span><p id="par0005" class="elsevierStylePara elsevierViewall">The direct carotid cavernous fistulas (dCCF) are high-flow shunts between the internal carotid artery (ICA) and cavernous sinus and are classified as type A carotid cavernous fistulas (CCF). Reconstructive techniques with preservation of ICA have replaced carotid artery sacrifice for occlusion of the shunt.<a class="elsevierStyleCrossRefs" href="#bib0080"><span class="elsevierStyleSup">1,2</span></a> Detachable coils, with or without stenting of ICA to cover the arterial defect, have been frequently used for treatment of dCCFs since the withdrawal of detachable balloons from the US market due to the leakage of the balloon valve.<a class="elsevierStyleCrossRefs" href="#bib0090"><span class="elsevierStyleSup">3,4</span></a> However, coils are associated with mass effect and recurrence can occur due to coil compaction.<a class="elsevierStyleCrossRef" href="#bib0100"><span class="elsevierStyleSup">5</span></a> Also, complete occlusion of the fistula with coils might be difficult to achieve due to the high flow in dCCFs and is associated with the risk of coil migration.<a class="elsevierStyleCrossRef" href="#bib0105"><span class="elsevierStyleSup">6</span></a> In such cases, deployment of covered stents in ICA is considered as an alternative for occlusion of dCCFs.<a class="elsevierStyleCrossRef" href="#bib0080"><span class="elsevierStyleSup">1</span></a> We present a case of dCCF with a tortuous intracranial ICA successfully treated by placement of a covered stent graft. We will also illustrate the technical challenges during the procedure.</p></span><span id="sec0010" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0030">Case presentation</span><p id="par0010" class="elsevierStylePara elsevierViewall">The patient is a 19-year-old male with history of gunshot wound to the face, complicated by left ICA injury. CT angiography showed a small pseudoaneurysm of the left ICA in the cavernous segment (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>, A). Repeat CT angiography 2 months after the injury demonstrated significant increase in size of the pseudoaneurysm with development of more prominent enhancement of the veins in the region, suggestive of an AV fistula (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>, B). Digital subtraction angiography (DSA) showed rapid shunting at the posterior cavernous segment of the left ICA into the left cavernous sinus and a 3.8<span class="elsevierStyleHsp" style=""></span>mm superiorly directed pseudoaneurysm arising approximately 2<span class="elsevierStyleHsp" style=""></span>mm from the ophthalmic origin. Due to the high-flow nature of the dCCF, coil embolization did not seem to be a suitable treatment option and a coronary stent graft was selected for occlusion of the shunt. The patient was started on dual antiplatelet therapy (DAPT) with Aspirin 325<span class="elsevierStyleHsp" style=""></span>mg and Plavix 75<span class="elsevierStyleHsp" style=""></span>mg one week prior to the procedure. It was decided to first stent across the dCCF, with the hope that this would straighten the vessel and provide more support for accessing the pseudoaneurysm. An Excelsior SL-10 microcatheter (Stryker Neurovascular, Fremont, California, USA) was advanced over a Synchro 2 microwire (Stryker Neurovascular, Fremont, California, USA) across the cavernous ICA and into the proximal left M2 segment. The microwire was removed and the SL-10 was exchanged over an exchange length Transend 014 wire (Stryker Neurovascular, Fremont, California, USA). A 4.8<span class="elsevierStyleHsp" style=""></span>mm<span class="elsevierStyleHsp" style=""></span>×<span class="elsevierStyleHsp" style=""></span>19<span class="elsevierStyleHsp" style=""></span>mm Graftmaster coronary stent graft (Abbott Vascular, Santa Clara, California, USA) was loaded onto the microwire and was advanced into the cavernous ICA. The balloon was inflated to a maximal pressure of 15 atmospheres and the stent was deployed without difficulty. Angiography demonstrated a tiny persistent fistula. To prevent endoleak, the stent balloon was removed and a 6<span class="elsevierStyleHsp" style=""></span>mm<span class="elsevierStyleHsp" style=""></span>×<span class="elsevierStyleHsp" style=""></span>12<span class="elsevierStyleHsp" style=""></span>mm angioplasty balloon was advanced over the Rx system into the mid stent. The balloon was inflated to a maximal pressure of 6 atmospheres, resulting in improved wall apposition of the stent. The balloon was removed, and angiography confirmed no residual fistula.</p><elsevierMultimedia ident="fig0005"></elsevierMultimedia><p id="par0015" class="elsevierStylePara elsevierViewall">Next, the ophthalmic pseudoaneurysm was coiled, using Penumbra Smart Coils (Penumbra Inc., Alameda, CA, USA), and the final angiography demonstrated no evidence of thromboembolic or hemorrhagic complication (<a class="elsevierStyleCrossRef" href="#fig0010">Fig. 2</a>, A, B) The patient was aroused from general anesthesia to his baseline neurologic status in stable condition. No immediate complications were encountered. After a month, the Aspirin 325<span class="elsevierStyleHsp" style=""></span>mg and Plavix were transitioned to Aspirin 81<span class="elsevierStyleHsp" style=""></span>mg and Apixaban that were continued for 6 months. The follow up DSA after 3 months showed no residual dCCF and no residual filling of the left ophthalmic artery pseudoaneurysm (<a class="elsevierStyleCrossRef" href="#fig0015">Fig. 3</a>, A, B).</p><elsevierMultimedia ident="fig0010"></elsevierMultimedia><elsevierMultimedia ident="fig0015"></elsevierMultimedia></span><span id="sec0015" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0035">Discussion</span><p id="par0020" class="elsevierStylePara elsevierViewall">Endovascular stent placement for management of a dCCF, Barrow type A, in the presence of a tortuous ICA is technically complicated and requires modified maneuvers for stent deployment. A suitable stent for this purpose should exhibit sufficient radial force to allow full apposition to the vessel wall without residual shunt, minimal recoil to avoid reduction in vessel diameter, and adequate longitudinal flexibility to permit easy navigation through a tortuous ICA.</p><p id="par0025" class="elsevierStylePara elsevierViewall">Redekop et al. published one of the early reports on feasibility and safety of using covered stent grafts for traumatic vascular lesions in skull base.<a class="elsevierStyleCrossRef" href="#bib0110"><span class="elsevierStyleSup">7</span></a> Kocer et al. in 2002 described the first experience with using a covered stent for treatment of a dCCF after a transsphenoidal surgery in a patient who was not a candidate for other treatment options.<a class="elsevierStyleCrossRef" href="#bib0115"><span class="elsevierStyleSup">8</span></a> Since then, the covered stents have been sporadically used in a single or combined approach with coiling of cavernous sinus, or after the failure of other methods for closing a dCCF.<a class="elsevierStyleCrossRef" href="#bib0100"><span class="elsevierStyleSup">5</span></a></p><p id="par0030" class="elsevierStylePara elsevierViewall">The covered stents are either self-expanding or balloon-expanding. Despite the higher flexibility and lower rates of vasospasm, vessel rupture and in-stent stenosis, the self-expanding stents have less radial force and, unlike the balloon-expanding stents that fully expand upon deployment, it takes a few days to several weeks for self-expanding stents to reach their maximum diameter. The self-expanding Symbiot covered stent (Boston Scientific, Natick, Massachusetts, USA) has been associated with late stent fracture in a case of large traumatic distal ICA pseudoaneurysm with a tortuous ICA.<a class="elsevierStyleCrossRef" href="#bib0120"><span class="elsevierStyleSup">9</span></a> Available covered stents are mainly designed for stenting the coronary arteries. The balloon-expanding Willis covered stent was introduced by MicroPort Medical Company (Shanghai, China) specifically for implantation in intracranial vessels. Although it was more flexible than other covered stents, it was not pliable enough to conform to the vessels with high curvature and was associated with stent detachment from the inflating balloon after multiple attempts for bypassing a tortuous ICA.<a class="elsevierStyleCrossRef" href="#bib0125"><span class="elsevierStyleSup">10</span></a> The balloon-expanding covered stents, such as Jostent coronary stent grafts (Abbott Vascular, Redwood City, California, USA), have sufficient radial strength to provide the desired intraluminal support in parent artery; however, their poor longitudinal flexibility leads to difficult stent delivery in tortuous vessels and increases the risk of vessel spasm, dissection and perforation due to the friction between the stent and vessel wall.<a class="elsevierStyleCrossRef" href="#bib0130"><span class="elsevierStyleSup">11</span></a> In a report by Lv et al. a group of 15 patients with intracranial vascular lesions, including 6 cases of dCCF, were selected for endovascular treatment by Jostent covered stent; however, the procedure was failed in 2 patients due to high tortuosity of ICA.<a class="elsevierStyleCrossRef" href="#bib0135"><span class="elsevierStyleSup">12</span></a> Another limitation is the size availability; the largest available diameter of the Jostent covered stents is 5<span class="elsevierStyleHsp" style=""></span>mm; therefore the procedure would be associated with higher risk of endoleak in vessels larger than 5<span class="elsevierStyleHsp" style=""></span>mm in diameter.<a class="elsevierStyleCrossRef" href="#bib0100"><span class="elsevierStyleSup">5</span></a></p><p id="par0035" class="elsevierStylePara elsevierViewall">Flow diverters are designed to occlude the aneurysm while preserving the patency of the covered branches and perforators. Several studies have shown successful occlusion of dCCFs using flow diverters in conjunction with coils or detachable balloons for dCCFs.<a class="elsevierStyleCrossRef" href="#bib0085"><span class="elsevierStyleSup">2</span></a> In a case report, Nadarajah et al. discussed the safety and efficacy of flow diverters as the only treatment for dCCFs. In their case, multiple flow diverters were placed with an overlapping technique to augment the metal coverage over the fistula.<a class="elsevierStyleCrossRef" href="#bib0080"><span class="elsevierStyleSup">1</span></a> While the flow diverters preserve the patency of the covered branches, there remains uncertainty regarding the efficacy of using the flow diverters alone for complete occlusion of a high flow dCCF.<a class="elsevierStyleCrossRef" href="#bib0085"><span class="elsevierStyleSup">2</span></a> To straighten a tortuous extracranial ICA, several techniques such as telescopic stent placement or neck extension have been proposed; however, these techniques are not applicable to a tortuous intracranial ICA.<a class="elsevierStyleCrossRefs" href="#bib0140"><span class="elsevierStyleSup">13,14</span></a> Our case was challenging due to tortuosity in the carotid siphon. Self-expanding segmented covered stents have been recently introduced for extracranial applications that are featuring higher flexibility and adoptability compared to one-piece stents.<a class="elsevierStyleCrossRefs" href="#bib0100"><span class="elsevierStyleSup">5,15</span></a> Hypothetically, if the segmented covered stents were available for placement in intracranial vasculature it could make a significant improvement in navigation and deployment of the covered stent in a tortuous intracranial ICA.</p></span><span id="sec0020" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0040">Conclusion</span><p id="par0040" class="elsevierStylePara elsevierViewall">Despite the lack of optimal flexibility, the balloon-expandable covered stents can be considered as an effective alternative treatment for high-flow dCCFs with a tortuous intracranial ICA not amenable to coil embolization.</p></span><span id="sec0025" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0045">Grant support</span><p id="par0045" class="elsevierStylePara elsevierViewall">This report was presented at the American Association of Neurological Surgeons meeting in April 2020, in Boston, MA, USA.</p></span><span id="sec0030" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0050">Conflict of interest</span><p id="par0050" class="elsevierStylePara elsevierViewall">The authors did not receive any grants and have no conflict of interest to disclose.</p></span></span>"
"textoCompletoSecciones" => array:1 [
"secciones" => array:12 [
0 => array:3 [
"identificador" => "xres1856387"
"titulo" => "Abstract"
"secciones" => array:1 [
0 => array:1 [
"identificador" => "abst0005"
]
]
]
1 => array:2 [
"identificador" => "xpalclavsec1614222"
"titulo" => "Keywords"
]
2 => array:3 [
"identificador" => "xres1856388"
"titulo" => "Resumen"
"secciones" => array:1 [
0 => array:1 [
"identificador" => "abst0010"
]
]
]
3 => array:2 [
"identificador" => "xpalclavsec1614223"
"titulo" => "Palabras clave"
]
4 => array:2 [
"identificador" => "sec0005"
"titulo" => "Introduction"
]
5 => array:2 [
"identificador" => "sec0010"
"titulo" => "Case presentation"
]
6 => array:2 [
"identificador" => "sec0015"
"titulo" => "Discussion"
]
7 => array:2 [
"identificador" => "sec0020"
"titulo" => "Conclusion"
]
8 => array:2 [
"identificador" => "sec0025"
"titulo" => "Grant support"
]
9 => array:2 [
"identificador" => "sec0030"
"titulo" => "Conflict of interest"
]
10 => array:2 [
"identificador" => "xack654279"
"titulo" => "Acknowledgement"
]
11 => array:1 [
"titulo" => "References"
]
]
]
"pdfFichero" => "main.pdf"
"tienePdf" => true
"fechaRecibido" => "2021-11-08"
"fechaAceptado" => "2022-04-29"
"PalabrasClave" => array:2 [
"en" => array:1 [
0 => array:4 [
"clase" => "keyword"
"titulo" => "Keywords"
"identificador" => "xpalclavsec1614222"
"palabras" => array:5 [
0 => "Carotid"
1 => "Cavernous"
2 => "Fistula"
3 => "Stent"
4 => "Covered"
]
]
]
"es" => array:1 [
0 => array:4 [
"clase" => "keyword"
"titulo" => "Palabras clave"
"identificador" => "xpalclavsec1614223"
"palabras" => array:5 [
0 => "Carótida"
1 => "Cavernosa"
2 => "Fístula"
3 => "Stent"
4 => "Cubierto"
]
]
]
]
"tieneResumen" => true
"resumen" => array:2 [
"en" => array:2 [
"titulo" => "Abstract"
"resumen" => "<span id="abst0005" class="elsevierStyleSection elsevierViewall"><p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Direct carotid cavernous fistulas (dCCF) are high-flow shunts between the internal carotid artery (ICA) and cavernous sinus and are commonly caused by traumatic injuries. Endovascular intervention using detachable coils, with or without stenting, is often the treatment of choice; however, migration or compaction of the coils can occur due to high-flow nature of dCCFs. Alternatively, deployment of a covered stent in ICA can be considered for treatment of dCCFs. We report a case of dCCF with tortuous intracranial ICA successfully treated by placement of a covered stent graft and we will illustrate the technical aspects of the procedure. In the presence of a tortuous ICA navigation and deployment of covered stents is technically complicated and requires modified maneuvers.</p></span>"
]
"es" => array:2 [
"titulo" => "Resumen"
"resumen" => "<span id="abst0010" class="elsevierStyleSection elsevierViewall"><p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">Las fístulas carótidas cavernosas directas (dCCF) son derivaciones de alto flujo entre la arteria carótida interna (ACI) y el seno cavernoso y suelen ser causadas por lesiones traumáticas. La intervención intravascular con espirales desmontables, con o sin stent, suele ser el tratamiento de elección; sin embargo, la migración o compactación de las bobinas puede ocurrir debido a la naturaleza de alto flujo de los dCCF. Alternativamente, se puede considerar el despliegue de un stent cubierto en la ACI para el tratamiento de dCCF. Presentamos un caso de dCCF con ACI intracraneal tortuosa tratada con éxito mediante la colocación de una endoprótesis cubierta e ilustraremos los aspectos técnicos del procedimiento. En presencia de una ACI tortuosa, la navegación y el despliegue de los stents cubiertos es técnicamente complicado y requiere maniobras modificadas.</p></span>"
]
]
"multimedia" => array:3 [
0 => array:7 [
"identificador" => "fig0005"
"etiqueta" => "Fig. 1"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr1.jpeg"
"Alto" => 498
"Ancho" => 1005
"Tamanyo" => 57341
]
]
"descripcion" => array:1 [
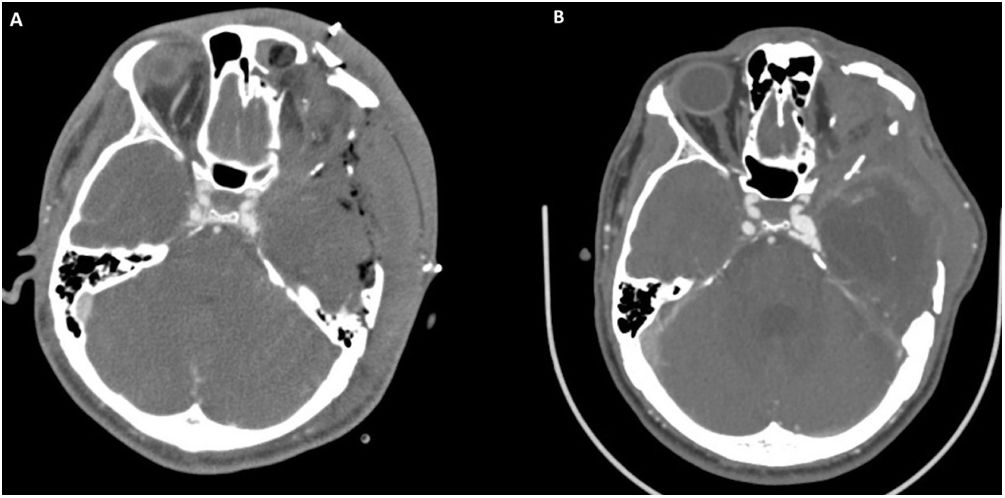
"en" => "<p id="spar0015" class="elsevierStyleSimplePara elsevierViewall">Initial CTA showing small pseudoaneurysm involving left posterior cavernous sinus (A) with significant increase in size on 2 months follow up CTA (B).</p>"
]
]
1 => array:7 [
"identificador" => "fig0010"
"etiqueta" => "Fig. 2"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr2.jpeg"
"Alto" => 996
"Ancho" => 2008
"Tamanyo" => 120565
]
]
"descripcion" => array:1 [
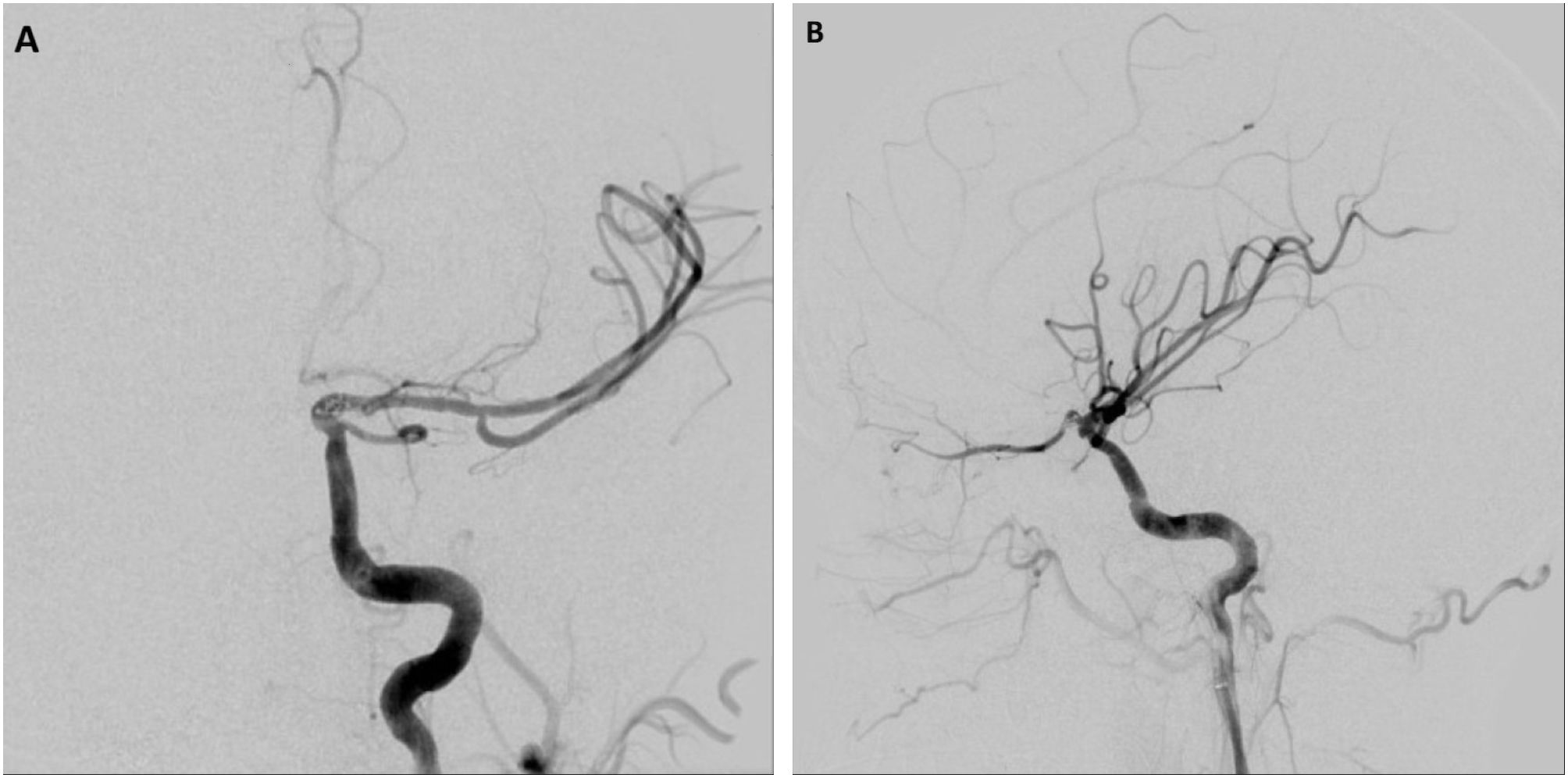
"en" => "<p id="spar0020" class="elsevierStyleSimplePara elsevierViewall">Immediate postoperative DSA AP (A) and lateral (B) views show a widely patent stent without residual arteriovenous shunt.</p>"
]
]
2 => array:7 [
"identificador" => "fig0015"
"etiqueta" => "Fig. 3"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr3.jpeg"
"Alto" => 773
"Ancho" => 1607
"Tamanyo" => 177474
]
]
"descripcion" => array:1 [
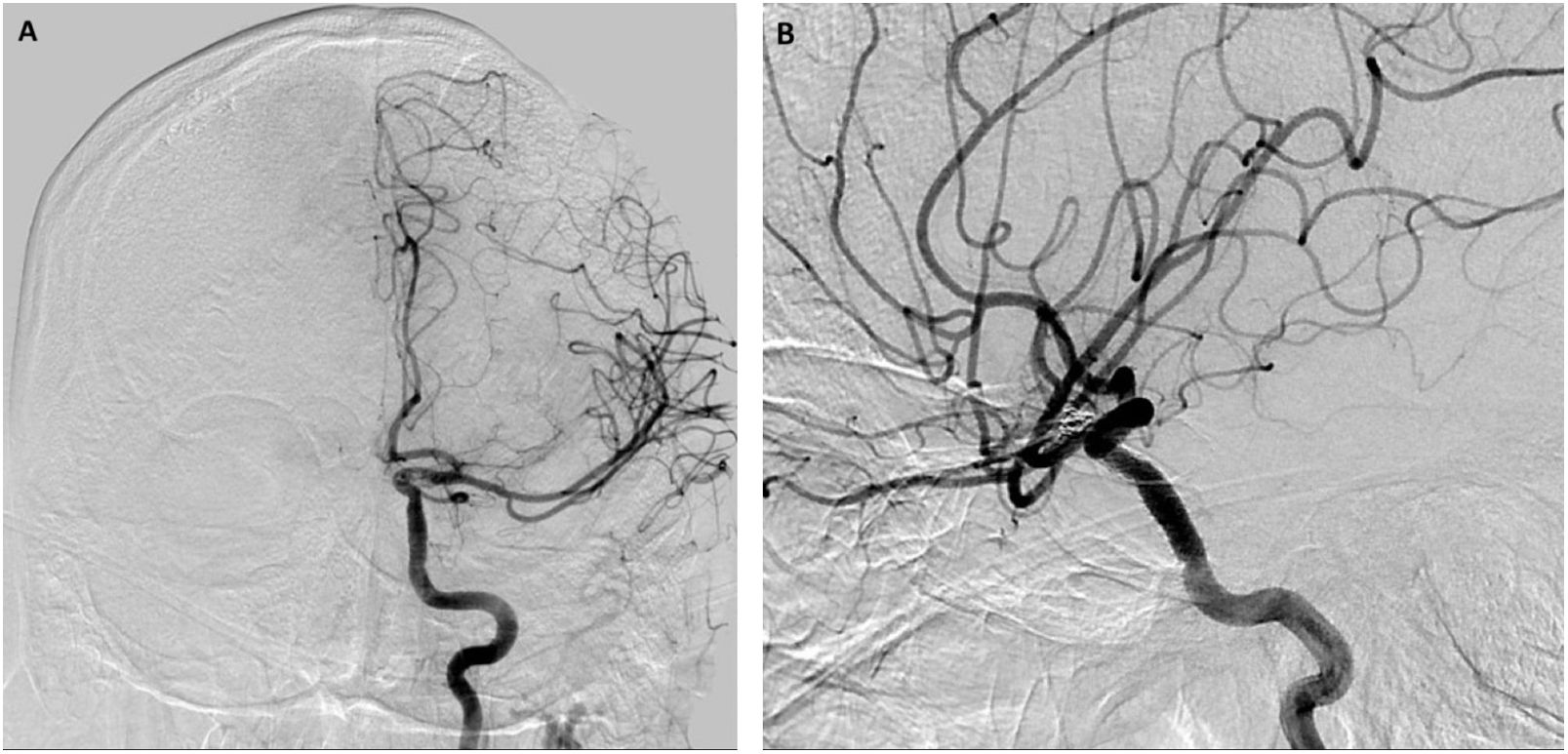
"en" => "<p id="spar0025" class="elsevierStyleSimplePara elsevierViewall">Follow up DSA AP (A) and lateral (B) views 3 months postoperatively shows no residual dCCF of the left cavernous ICA and no residual filling of the left ophthalmic artery pseudoaneurysm.</p>"
]
]
]
"bibliografia" => array:2 [
"titulo" => "References"
"seccion" => array:1 [
0 => array:2 [
"identificador" => "bibs0015"
"bibliografiaReferencia" => array:15 [
0 => array:3 [
"identificador" => "bib0080"
"etiqueta" => "1"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Treatment of a traumatic carotid–cavernous fistula by the sole use of a flow diverting stent"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:4 [
0 => "M. Nadarajah"
1 => "M. Power"
2 => "B. Barry"
3 => "J. Wenderoth"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1136/neurintsurg-2011-010000"
"Revista" => array:4 [
"tituloSerie" => "J NeuroIntervent Surg"
"fecha" => "2012"
"volumen" => "4"
"paginaInicial" => "e1"
]
]
]
]
]
]
1 => array:3 [
"identificador" => "bib0085"
"etiqueta" => "2"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Flow diverters as useful adjunct to traditional endovascular techniques in treatment of direct carotid-cavernous fistulas"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:6 [
0 => "C.S. Ogilvy"
1 => "R. Motiei-Langroudi"
2 => "M. Ghorbani"
3 => "C.J. Griessenauer"
4 => "A.Y. Alturki"
5 => "A.J. Thomas"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/j.wneu.2017.06.113"
"Revista" => array:6 [
"tituloSerie" => "World Neurosurg"
"fecha" => "2017"
"volumen" => "105"
"paginaInicial" => "812"
"paginaFinal" => "817"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/28647659"
"web" => "Medline"
]
]
]
]
]
]
]
]
2 => array:3 [
"identificador" => "bib0090"
"etiqueta" => "3"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Endovascular techniques for treatment of carotid-cavernous fistula"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:3 [
0 => "J.J. Gemmete"
1 => "S.A. Ansari"
2 => "D.M. Gandhi"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1097/WNO.0b013e3181989fc0"
"Revista" => array:6 [
"tituloSerie" => "J Neuroophthalmol"
"fecha" => "2009"
"volumen" => "29"
"paginaInicial" => "62"
"paginaFinal" => "71"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/19458580"
"web" => "Medline"
]
]
]
]
]
]
]
]
3 => array:3 [
"identificador" => "bib0095"
"etiqueta" => "4"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "The evolution of endovascular treatment of carotid cavernous fistulas: a single-center experience"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:4 [
0 => "A.F. Ducruet"
1 => "F.C. Albuquerque"
2 => "R.W. Crowley"
3 => "C.G. McDougall"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/j.wneu.2013.02.033"
"Revista" => array:6 [
"tituloSerie" => "World Neurosurg"
"fecha" => "2013"
"volumen" => "80"
"paginaInicial" => "538"
"paginaFinal" => "548"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/23402868"
"web" => "Medline"
]
]
]
]
]
]
]
]
4 => array:3 [
"identificador" => "bib0100"
"etiqueta" => "5"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "A novel fully covered segmented irradiation stent for the palliation of malignant dysphagia"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:2 [
0 => "C. Wang"
1 => "J.-H. Guo"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/j.brachy.2018.04.033"
"Revista" => array:4 [
"tituloSerie" => "Brachytherapy"
"fecha" => "2018"
"volumen" => "17"
"paginaInicial" => "S27"
]
]
]
]
]
]
5 => array:3 [
"identificador" => "bib0105"
"etiqueta" => "6"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "High-flow, small-hole arteriovenous fistulas: treatment with electrodetachable coils"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:5 [
0 => "G. Guglielmi"
1 => "F. Viñuela"
2 => "G. Duckwiler"
3 => "J. Dion"
4 => "A. Stocker"
]
]
]
]
]
"host" => array:1 [
0 => array:1 [
"Revista" => array:6 [
"tituloSerie" => "Am J Neuroradiol"
"fecha" => "1995"
"volumen" => "16"
"paginaInicial" => "325"
"paginaFinal" => "328"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/7726080"
"web" => "Medline"
]
]
]
]
]
]
]
]
6 => array:3 [
"identificador" => "bib0110"
"etiqueta" => "7"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Treatment of traumatic aneurysms and arteriovenous fistulas of the skull base by using endovascular stents"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:3 [
0 => "G. Redekop"
1 => "T. Marotta"
2 => "A. Weill"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.3171/jns.2001.95.3.0412"
"Revista" => array:6 [
"tituloSerie" => "J Neurosurg"
"fecha" => "2001"
"volumen" => "95"
"paginaInicial" => "412"
"paginaFinal" => "419"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/11565861"
"web" => "Medline"
]
]
]
]
]
]
]
]
7 => array:3 [
"identificador" => "bib0115"
"etiqueta" => "8"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Treatment of iatrogenic internal carotid artery laceration and carotid cavernous fistula with endovascular stent-graft placement"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:6 [
0 => "N. Kocer"
1 => "O. Kizilkilic"
2 => "S. Albayram"
3 => "I. Adaletli"
4 => "F. Kantarci"
5 => "C. Islak"
]
]
]
]
]
"host" => array:1 [
0 => array:1 [
"Revista" => array:6 [
"tituloSerie" => "Am J Neuroradiol"
"fecha" => "2002"
"volumen" => "23"
"paginaInicial" => "442"
"paginaFinal" => "446"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/11901015"
"web" => "Medline"
]
]
]
]
]
]
]
]
8 => array:3 [
"identificador" => "bib0120"
"etiqueta" => "9"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Stent fracture after endoluminal repair of a carotid artery pseudoaneurysm"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:5 [
0 => "J.-P.P.M. de Vries"
1 => "R.W. Meijer"
2 => "J.C. van den Berg"
3 => "J.M.R. Meijer"
4 => "E.D.W.M. van de Pavoordt"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1583/05-1597.1"
"Revista" => array:6 [
"tituloSerie" => "J Endovasc Ther"
"fecha" => "2005"
"volumen" => "12"
"paginaInicial" => "612"
"paginaFinal" => "615"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/16212463"
"web" => "Medline"
]
]
]
]
]
]
]
]
9 => array:3 [
"identificador" => "bib0125"
"etiqueta" => "10"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Procedure-related complication of Willis covered stent in the treatment of blood blister-like aneurysm: stent detachment from dilating balloon"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:4 [
0 => "Y. Zhang"
1 => "Y. Zhang"
2 => "F. Liang"
3 => "C. Jiang"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.3389/fneur.2017.00639"
"Revista" => array:3 [
"tituloSerie" => "Front Neurol"
"fecha" => "2017"
"paginaInicial" => "8"
]
]
]
]
]
]
10 => array:3 [
"identificador" => "bib0130"
"etiqueta" => "11"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Angiographic follow-up of traumatic carotid cavernous fistulas treated with endovascular stent graft placement"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:5 [
0 => "E. Archondakis"
1 => "G. Pero"
2 => "L. Valvassori"
3 => "E. Boccardi"
4 => "G. Scialfa"
]
]
]
]
]
"host" => array:1 [
0 => array:1 [
"Revista" => array:6 [
"tituloSerie" => "Am J Neuroradiol"
"fecha" => "2007"
"volumen" => "28"
"paginaInicial" => "342"
"paginaFinal" => "347"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/17297009"
"web" => "Medline"
]
]
]
]
]
]
]
]
11 => array:3 [
"identificador" => "bib0135"
"etiqueta" => "12"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Intracranial pseudoaneurysms, fusiform aneurysms and carotid-cavernous fistulas"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:6 [
0 => "X. Lv"
1 => "C. Jiang"
2 => "Y. Li"
3 => "M. Lv"
4 => "J. Zhang"
5 => "Z. Wu"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1177/159101990801400409"
"Revista" => array:5 [
"tituloSerie" => "Intervent Neuroradiol"
"fecha" => "2008"
"volumen" => "14"
"paginaInicial" => "435"
"paginaFinal" => "440"
]
]
]
]
]
]
12 => array:3 [
"identificador" => "bib0140"
"etiqueta" => "13"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Endovascular remodeling of tortuous cervical segments of the internal carotid artery that hinder the management of complex intracranial aneurysms"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:4 [
0 => "M.A. Zenteno"
1 => "J.A. Santos-Franco"
2 => "L.R. Moscote-Salazar"
3 => "Á. Lee"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.2478/romneu-2013-0008"
"Revista" => array:5 [
"tituloSerie" => "Roman Neurosurg"
"fecha" => "2013"
"volumen" => "20"
"paginaInicial" => "249"
"paginaFinal" => "259"
]
]
]
]
]
]
13 => array:3 [
"identificador" => "bib0145"
"etiqueta" => "14"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Use of simple neck extension to improve guiding catheter accessibility in tortuous cervical internal carotid artery for endovascular embolization of intracranial aneurysm: a technical note"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:5 [
0 => "M. Takata"
1 => "H. Fukuda"
2 => "M. Kinosada"
3 => "K. Miyake"
4 => "K. Murao"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/j.wneu.2017.06.023"
"Revista" => array:6 [
"tituloSerie" => "World Neurosurg"
"fecha" => "2017"
"volumen" => "105"
"paginaInicial" => "529"
"paginaFinal" => "533"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/28619490"
"web" => "Medline"
]
]
]
]
]
]
]
]
14 => array:3 [
"identificador" => "bib0150"
"etiqueta" => "15"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "A comparison of a fully covered and an uncovered segmented biodegradable esophageal stent in a porcine model: preclinical evaluation of degradation, complications, and tissue reactions"
"autores" => array:1 [
0 => array:2 [
"etal" => true
"autores" => array:6 [
0 => "Y. Feng"
1 => "C. Jiao"
2 => "Y. Cao"
3 => "Y. Zhao"
4 => "Y. Chen"
5 => "L. Fang"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1155/2016/8690858"
"Revista" => array:5 [
"tituloSerie" => "Gastroenterol Res Pract"
"fecha" => "2016"
"volumen" => "2016"
"paginaInicial" => "1"
"paginaFinal" => "7"
]
]
]
]
]
]
]
]
]
]
"agradecimientos" => array:1 [
0 => array:4 [
"identificador" => "xack654279"
"titulo" => "Acknowledgement"
"texto" => "<p id="par0055" class="elsevierStylePara elsevierViewall">The authors are grateful to Ms. Margaret Sten from the University of California San Diego for assisting them in editing the manuscript.</p>"
"vista" => "all"
]
]
]
"idiomaDefecto" => "en"
"url" => "/11301473/0000003400000002/v1_202303021130/S1130147322000586/v1_202303021130/en/main.assets"
"Apartado" => array:4 [
"identificador" => "392"
"tipo" => "SECCION"
"es" => array:2 [
"titulo" => "Casos Clínicos"
"idiomaDefecto" => true
]
"idiomaDefecto" => "es"
]
"PDF" => "https://static.elsevier.es/multimedia/11301473/0000003400000002/v1_202303021130/S1130147322000586/v1_202303021130/en/main.pdf?idApp=UINPBA00004B&text.app=https://www.revistaneurocirugia.com/"
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S1130147322000586?idApp=UINPBA00004B"
]