Traumatic subdural haematomas often require emergency surgical evacuation. Spontaneous resolution of traumatic acute subdural haematomas (TASDH) is under-reported. Two patients are described with spontaneous resolution of TASDH correlating with previous reports. A discussion is presented on the clinical, pathological and radiological features of TASDH.
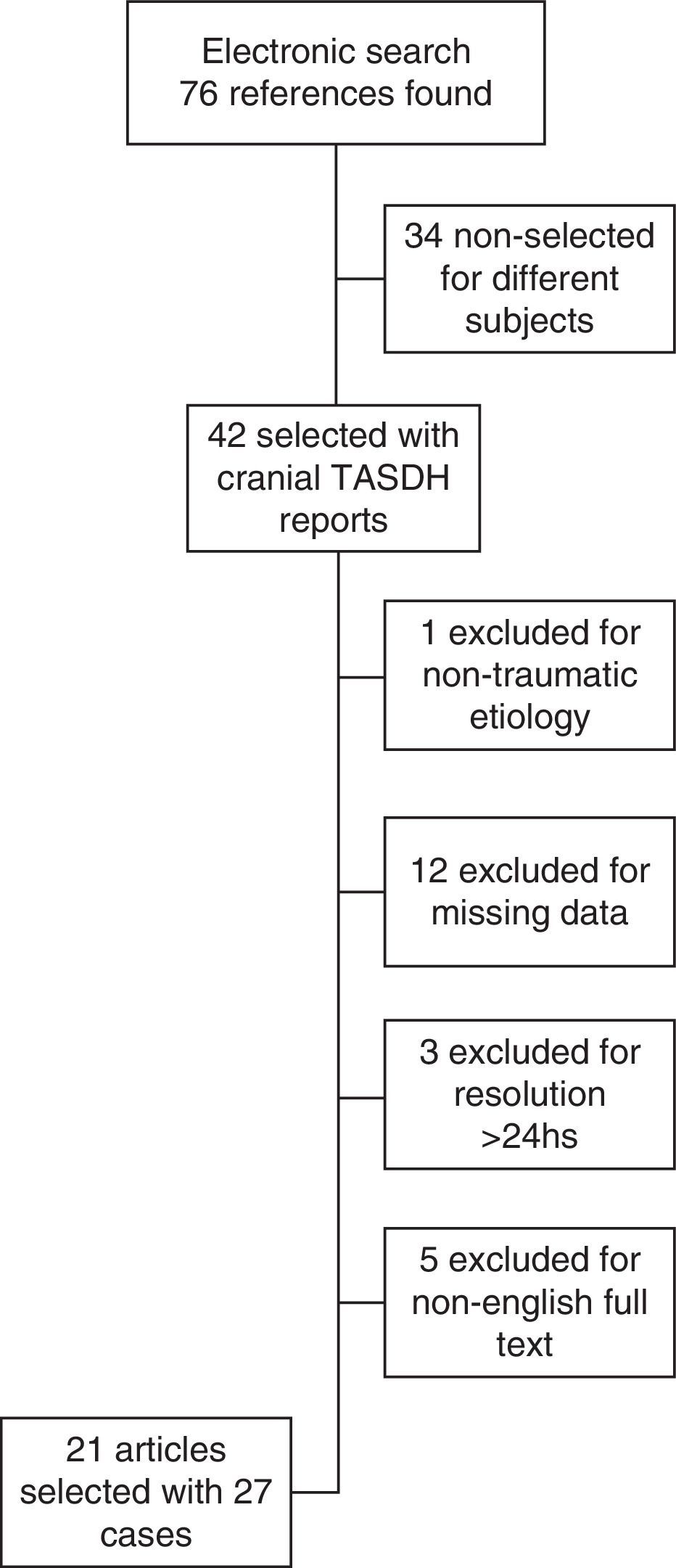
MethodsA review of the literature was performed using PubMed (Medline), Embase, and Cochrane Library for similar cases.
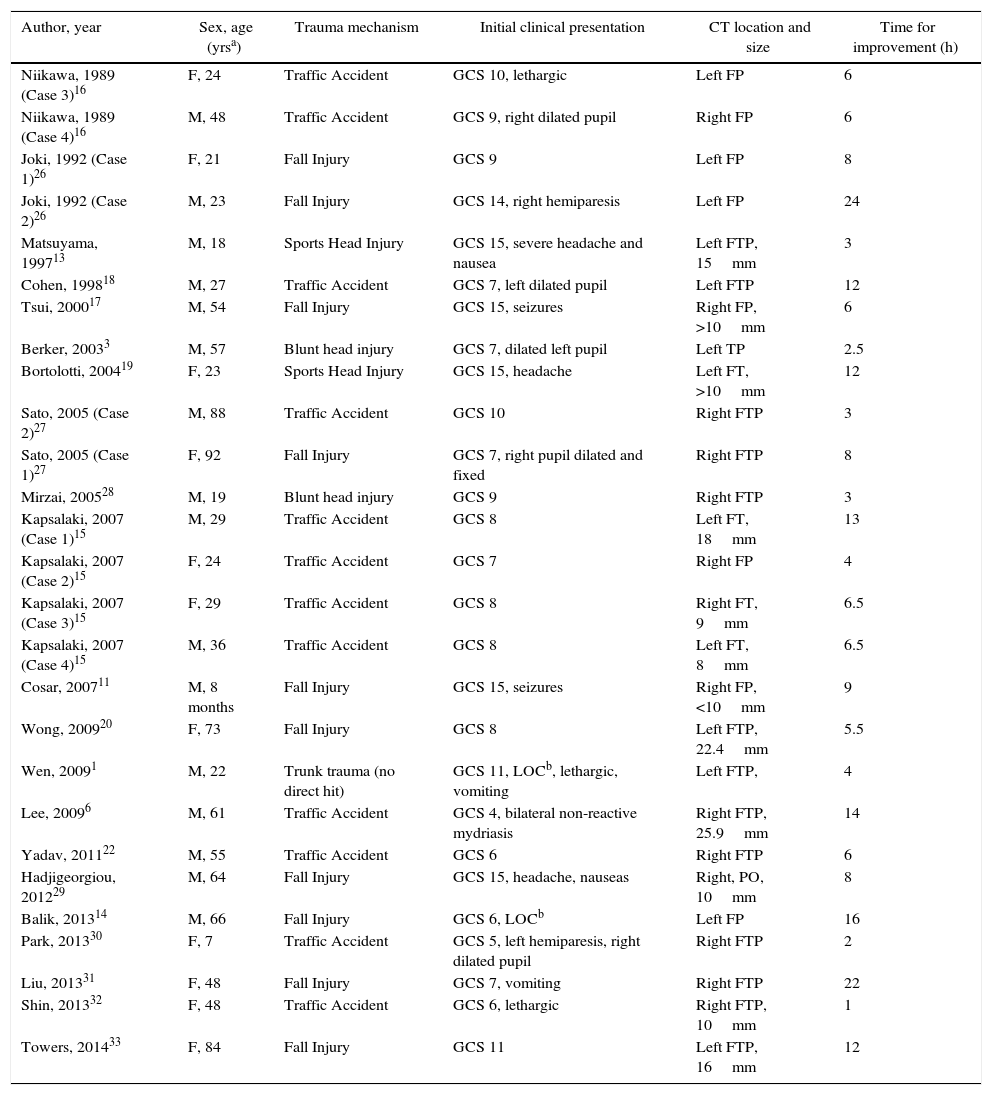
ResultsA total 21 articles were included, involving 27 cases well detailed of TASDH with spontaneous resolution or neurological and radiological improvement in less than 24h.
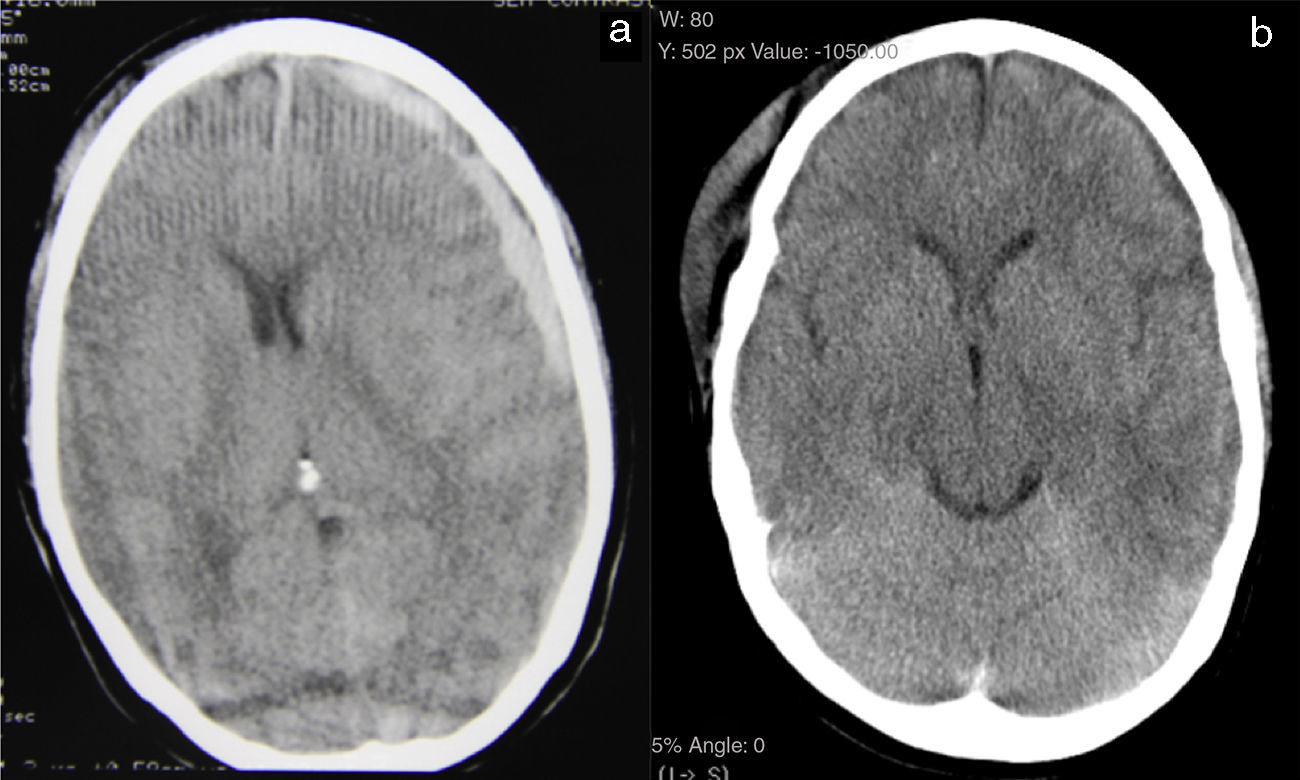
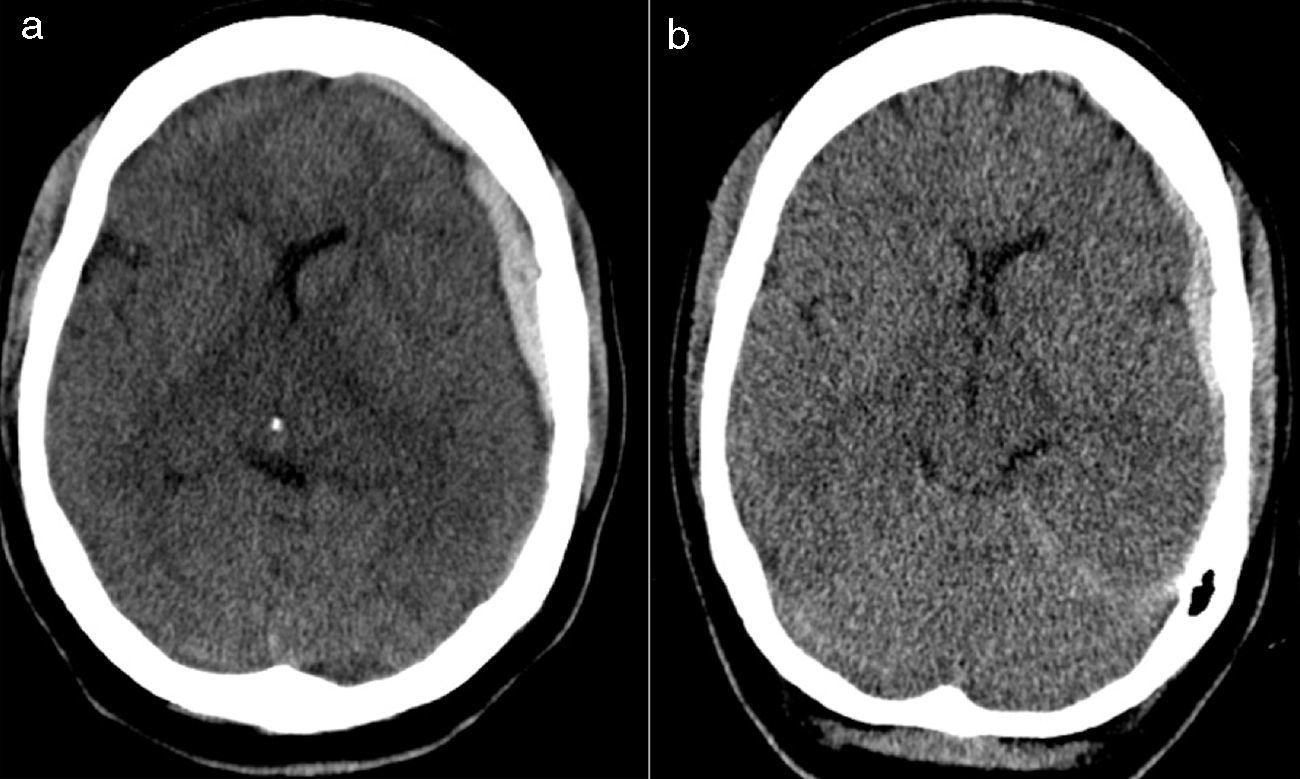
ConclusionsThere are two main mechanisms for the spontaneous resolution of acute subdural haematomas: dilution in subarachnoid space and redistribution of the haematoma in the subdural space. The primary radiological characteristic of these lesions is a hypodense rim on the outer surface of the clot. Spontaneous resolution of TASDH is unusual. Clinical and radiological surveillance is essential for appropriate management of these patients.
Los hematomas subdurales agudos traumáticos (HSDAT) requieren tratamiento quirúrgico de urgencia. Muy raras veces se describen casos de resolución espontánea de HSDAT. Describimos 2 casos de resolución espontánea de HSDAT y revisamos la bibliografía pertinente. Se discuten los aspectos clínicos, patológicos y radiológicos de resolución espontánea de HSDAT.
MétodosRevisamos la literatura en Pubmed (Medline), Embase y Cochrane Library en busca de casos similares.
ResultadosSe incluyeron 21 artículos con 27 casos bien detallados de HSDAT con resolución espontánea o mejora clínica y radiológica en 24h.
ConclusionesExisten 2 mecanismos principales para la resolución espontánea de hematomas subdurales agudos: la dilución en el espacio subaracnoideo y la redistribución del hematoma en el espacio subdural. La principal característica radiológica de estas lesiones es una cerco hipodenso en la superficie exterior del coágulo. La resolución espontánea de HSDAT es rara. La vigilancia clínica y radiológica es esencial para el manejo adecuado de estos pacientes.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.