To analyse the radiological outcomes in the long term of unstable thoracic and lumbar fractures treated through percutaneous surgery.
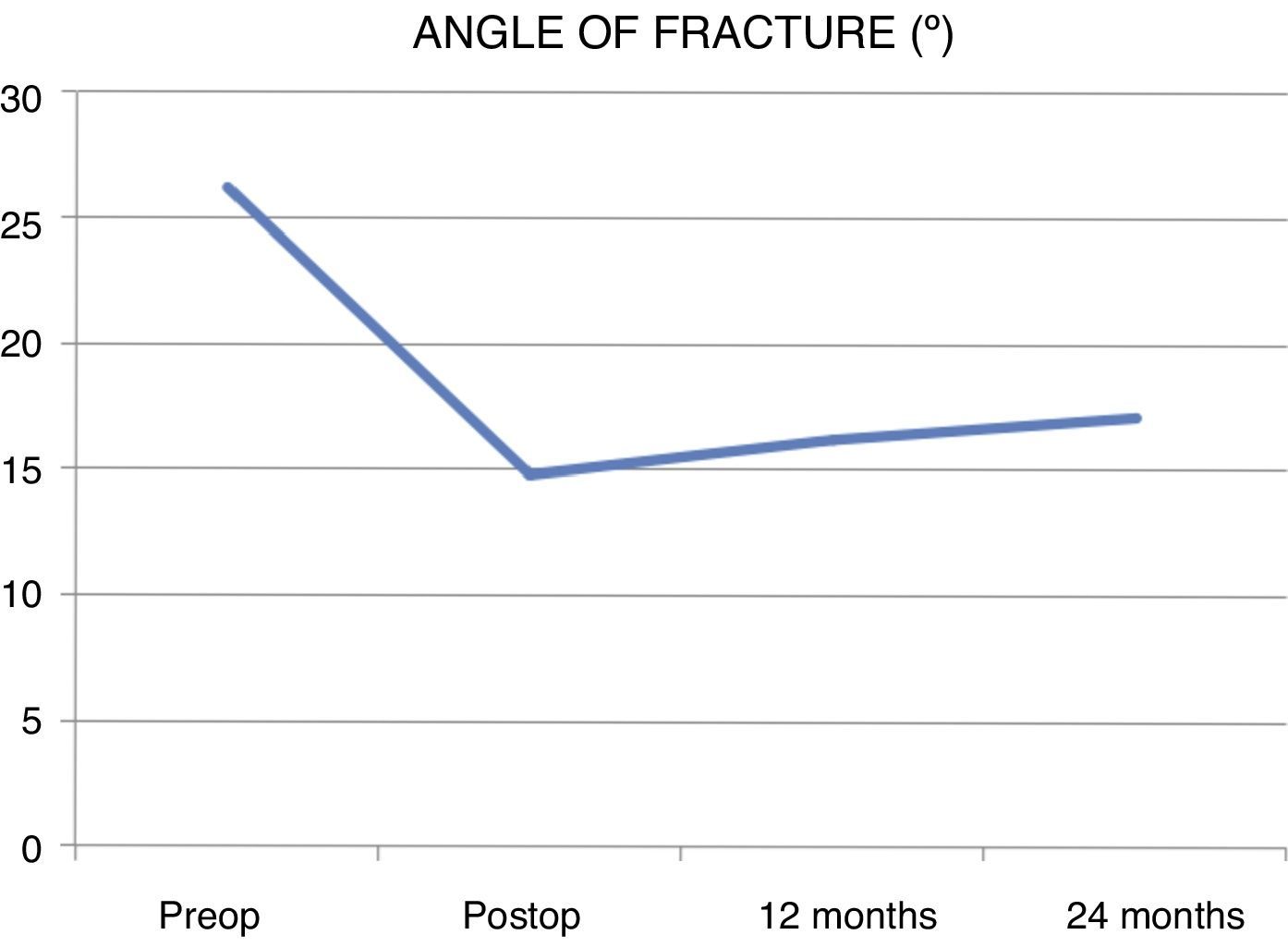
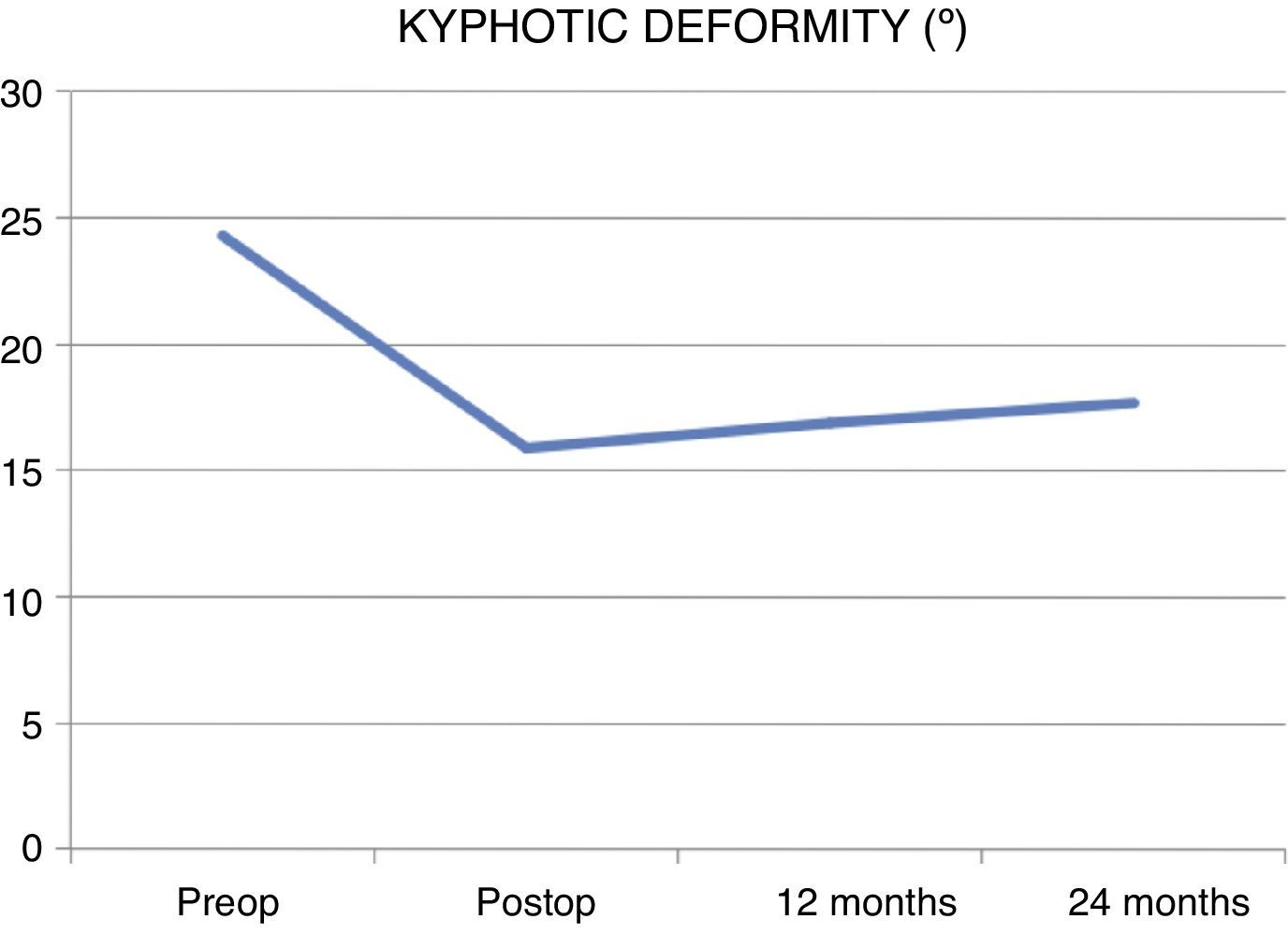
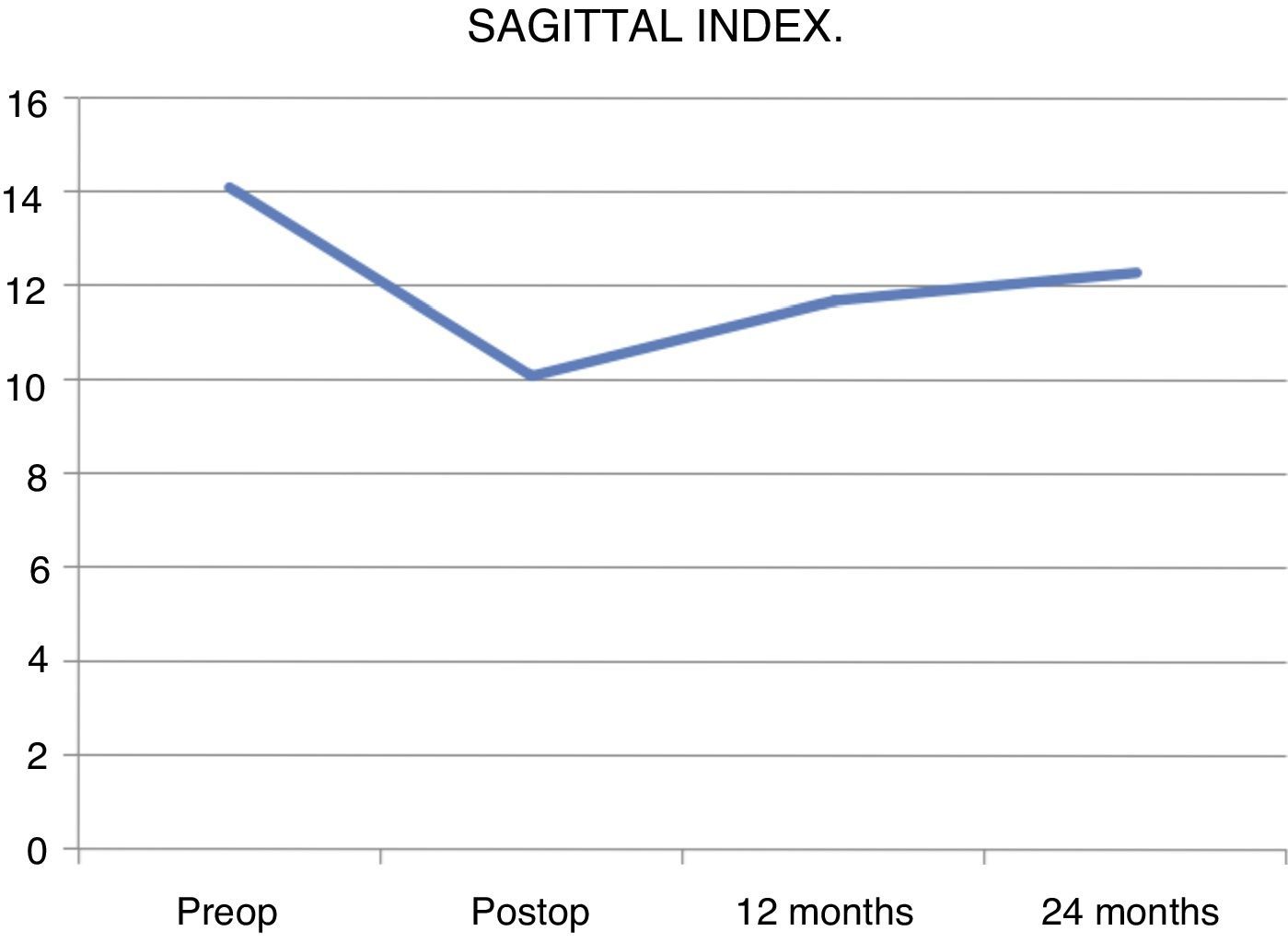
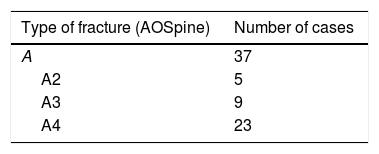
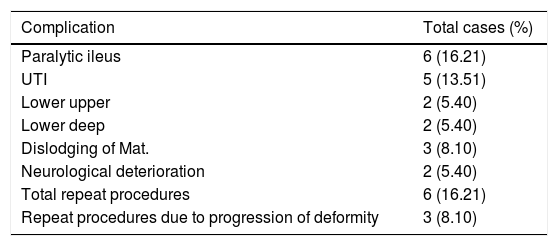
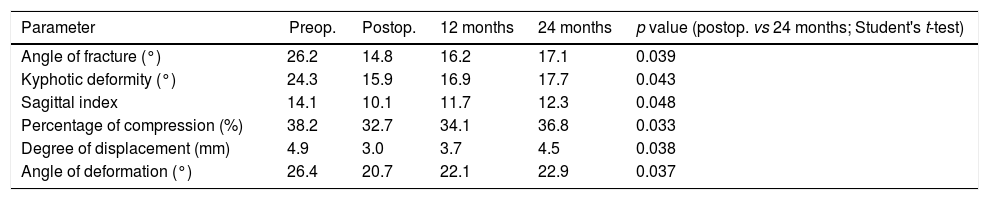
Material and methodsRetrospective review of a series of patients with unstable thoracic and lumbar fractures treated with percutaneous minimally invasive surgery between 2010 and 2015 in three different hospital centres. Six radiological parameters were measured annually during a 2-year period: Fracture angle, kyphotic deformity, sagittal index, percentage of compression, degree of displacement and deformation angle.
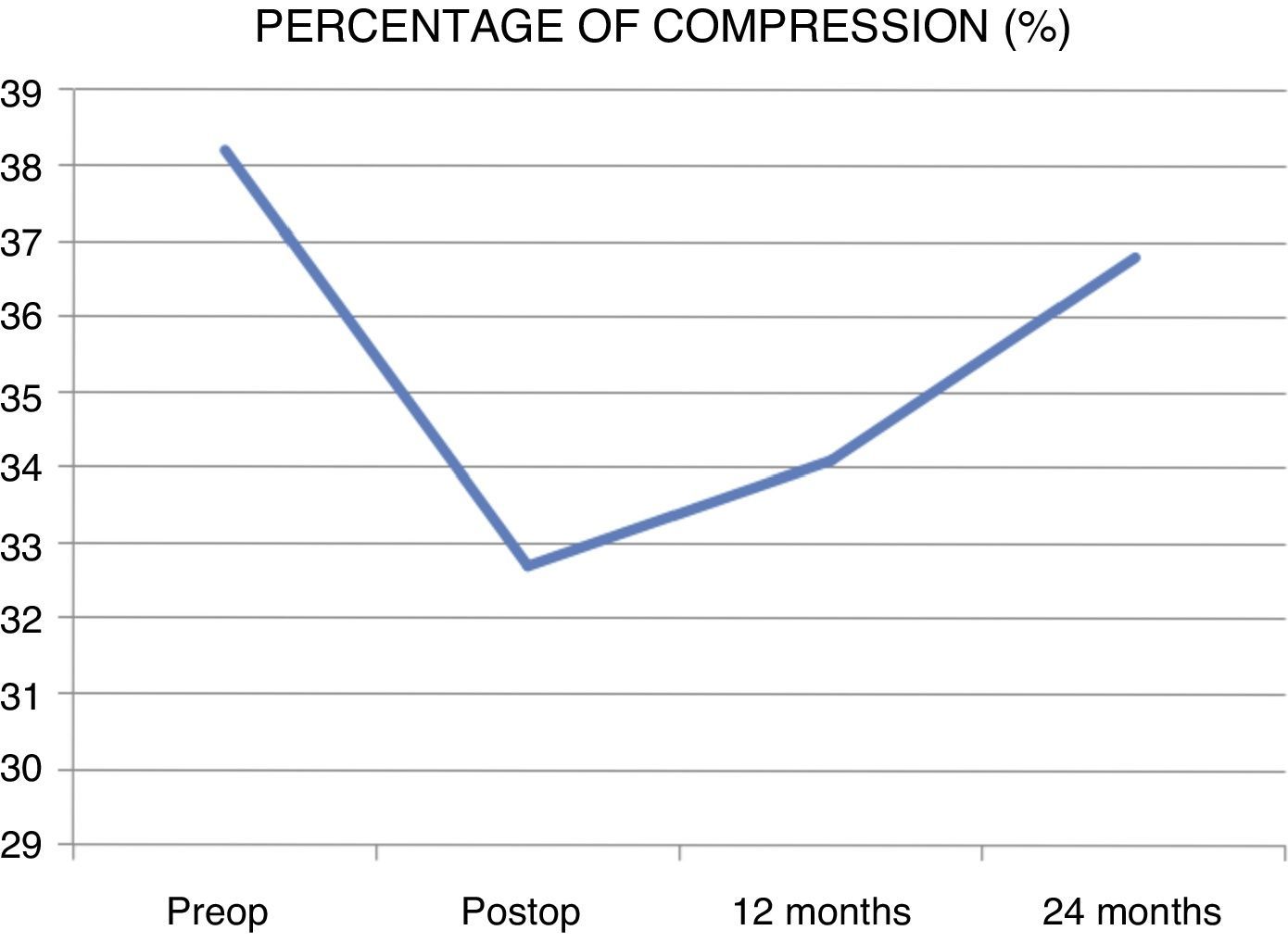
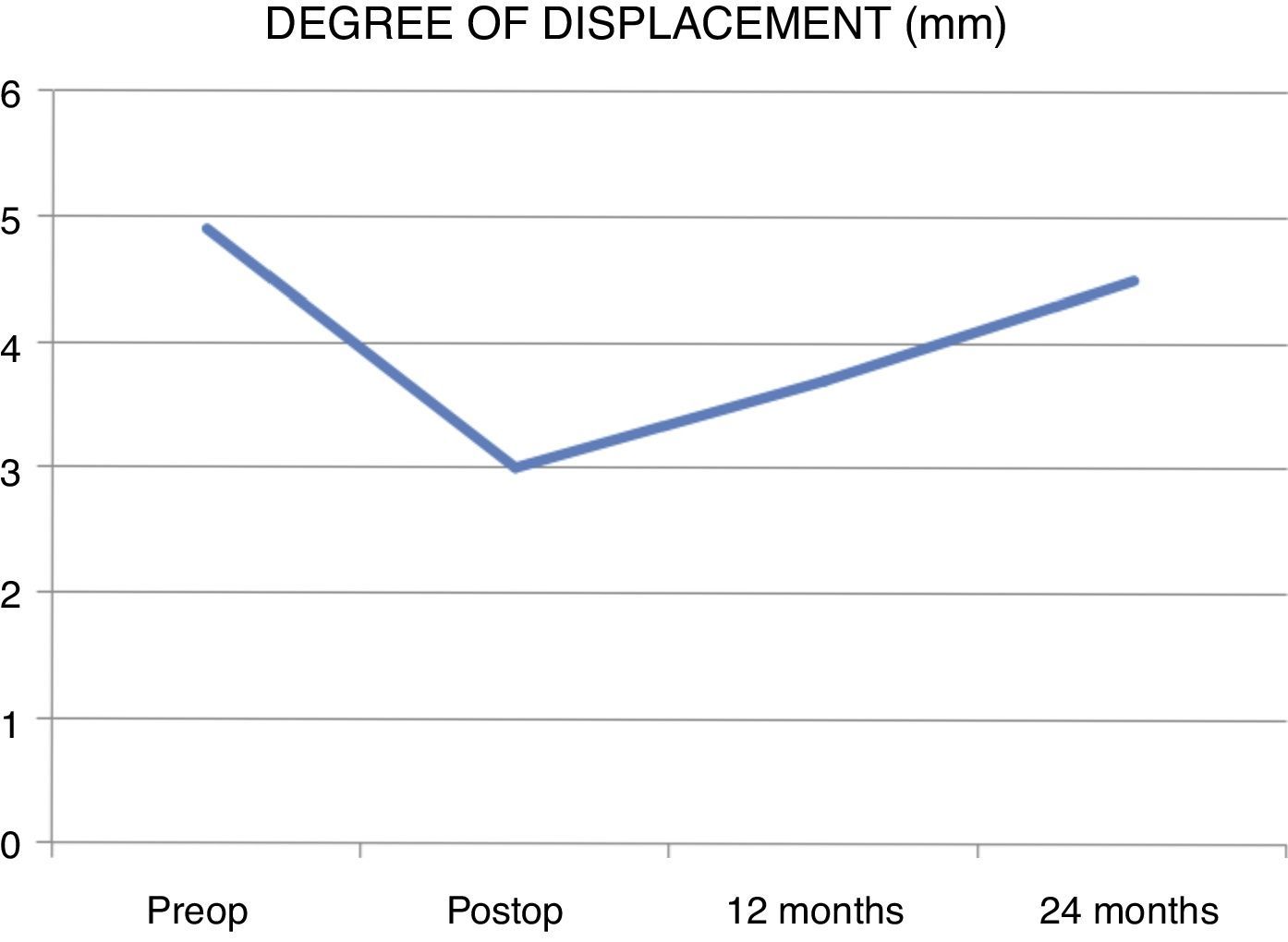
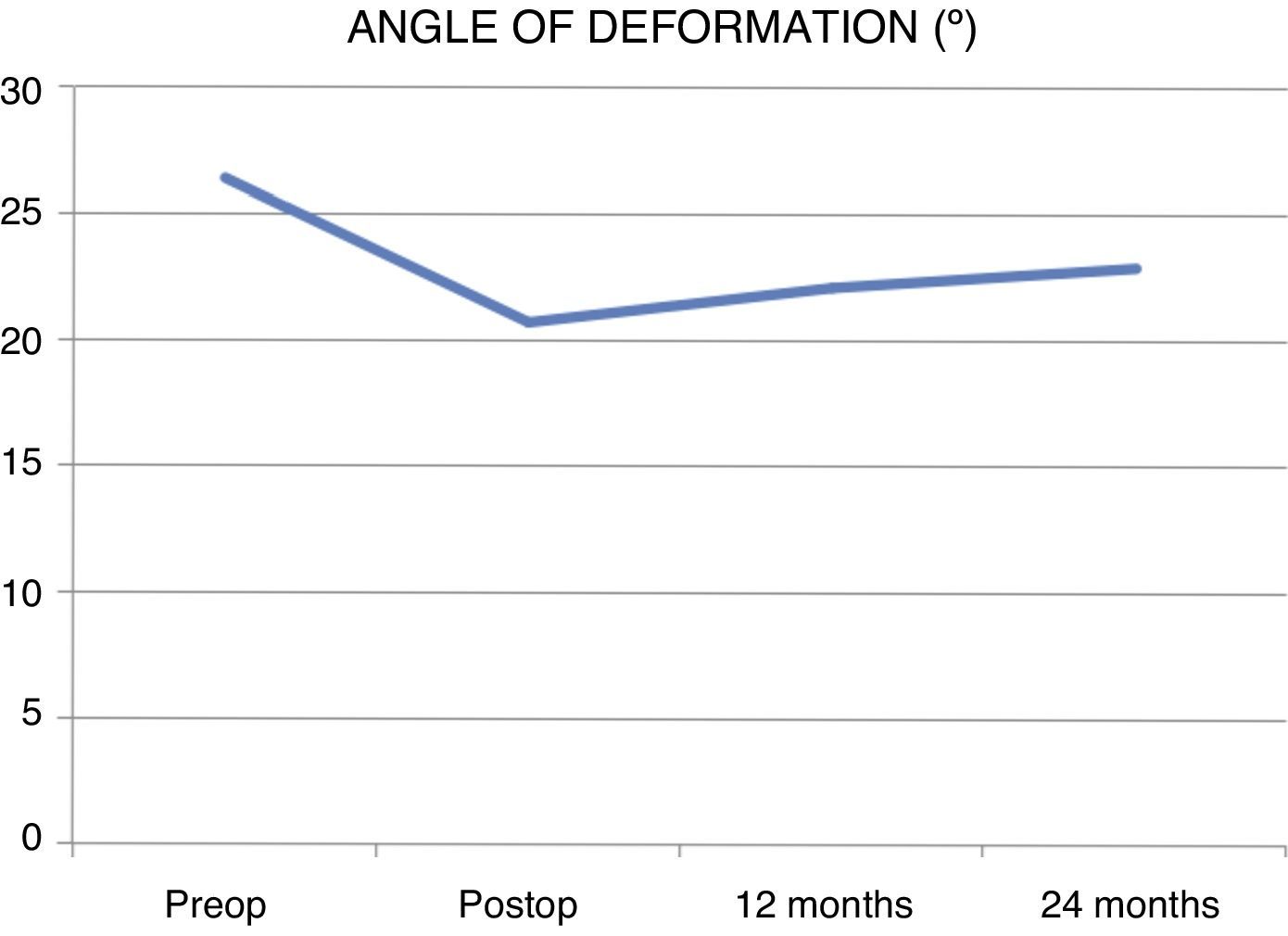
ResultsA total of 37 patients were included with a median age of 41.3 years and a median follow-up period of 2.2 years. Fracture angle rose from 14.8 to 17.1 (increase of 15.54%), kyphotic deformity from 15.9 to 17.7 (increase of 11.32%), sagittal index from 10.1 to 12.3 (increase of 21.78%), percentage of compression from 32.7% to 36.8% (increase of 12.53%), degree of displacement from 3.0mm to 4.4mm (increase of 50%) and deformation angle from 20.7 to 22.9 (increase of 10.62%).
ConclusionsAll the radiological parameters studied lost correction throughout the 24 months of follow-up; the degree of displacement and the sagittal index were the most marked. Nevertheless, the greatest loss of correction occurred in the first postoperative year, the parameters then stabilised over the 24 months of follow up. We routinely recommend the measurement of all previous parameters for the follow up of unstable thoracic and lumbar fractures treated through percutaneous surgery.
Analizar la evolución radiológica a largo plazo de las fracturas inestables torácicas y lumbares tratadas mediante cirugía percutánea.
Material y métodosSerie retrospectiva de una serie de casos con fracturas inestables torácicas y lumbares sin clínica neurológica tratadas mediante cirugía percutánea entre el 2010 y 2015 en 3 hospitales diferentes. Se midieron 6 parámetros radiológicos anualmente durante un período de 2años: ángulo fractuario, deformidad cifótica, índice sagital, porcentaje de compresión, grado de desplazamiento y ángulo de deformación.
ResultadosSe incluyeron un total de 37 pacientes de 41,3años de media, con un período de seguimiento medio de 2,2años. El ángulo fractuario pasó de 14,8 a 17,1° (incremento del 15,54%), la deformidad cifótica de 15,9 a 17,7° (incremento del 11,32%), el índice sagital de 10,1 a 12,3 (incremento del 21,78%), el porcentaje de compresión del 32,7 al 36,8% (incremento del 12,53%), el grado de desplazamiento de 3,0 a 4,5mm (incremento del 50%) y el ángulo de deformación de 20,7 a 22,9° (incremento del 10,62%).
ConclusionesTodos los parámetros radiológicos estudiados perdieron corrección a lo largo de los 24meses de seguimiento, siendo el grado de desplazamiento y el índice sagital los más marcados. Sin embargo, la mayor parte de la pérdida de corrección ocurre en el primer año postoperatorio, estabilizándose los parámetros posteriormente hasta los 24meses de seguimiento. Recomendamos la medición de todos los parámetros previos de rutina para el seguimiento de las fracturas inestables torácicas y lumbares tratadas mediante cirugía percutánea.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.