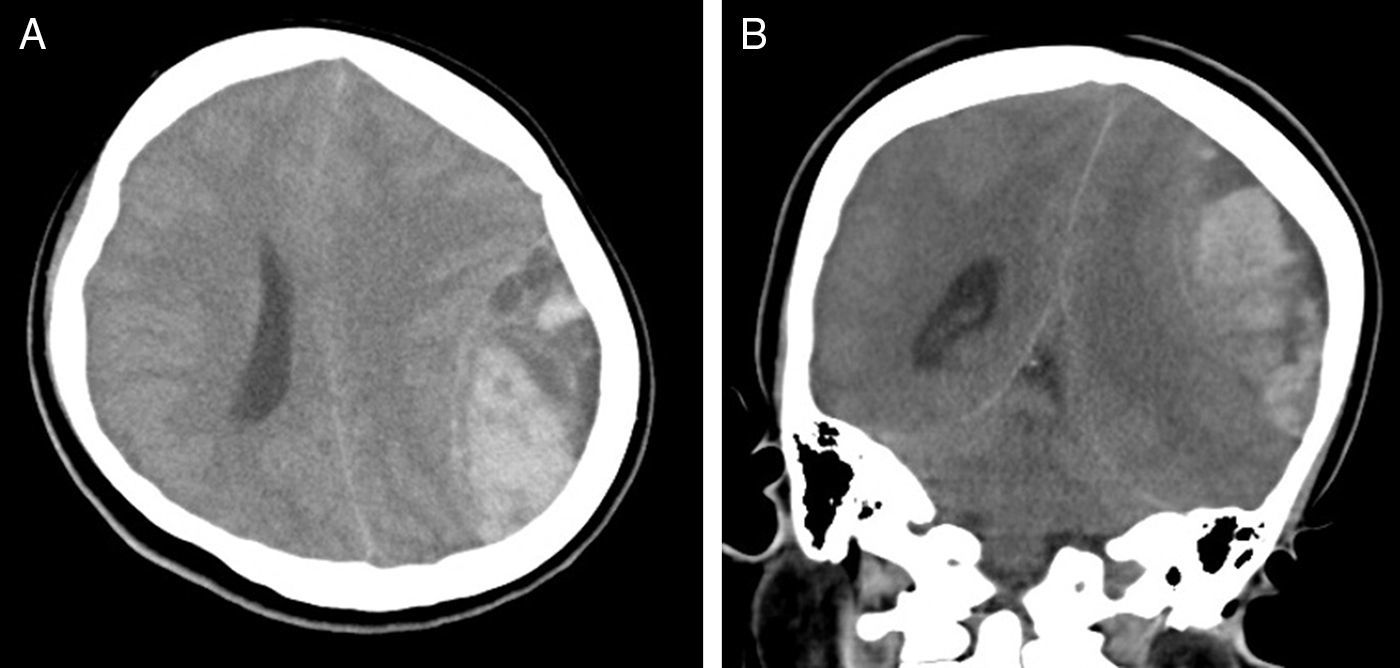
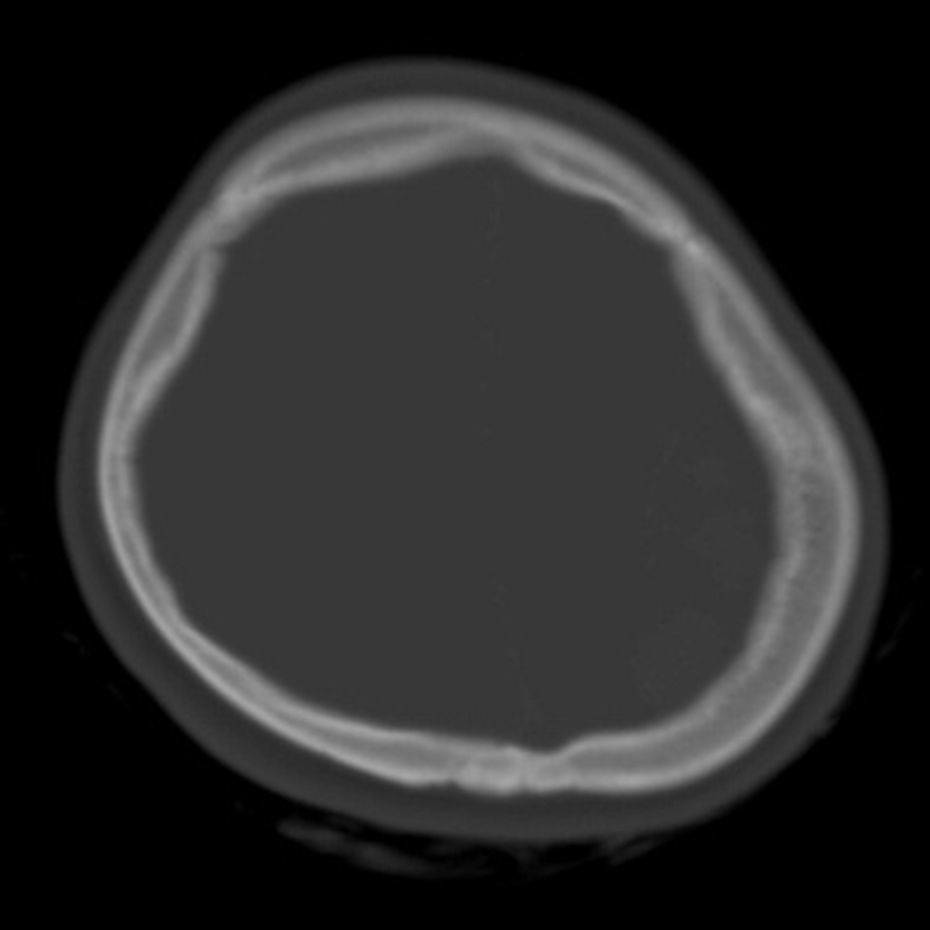
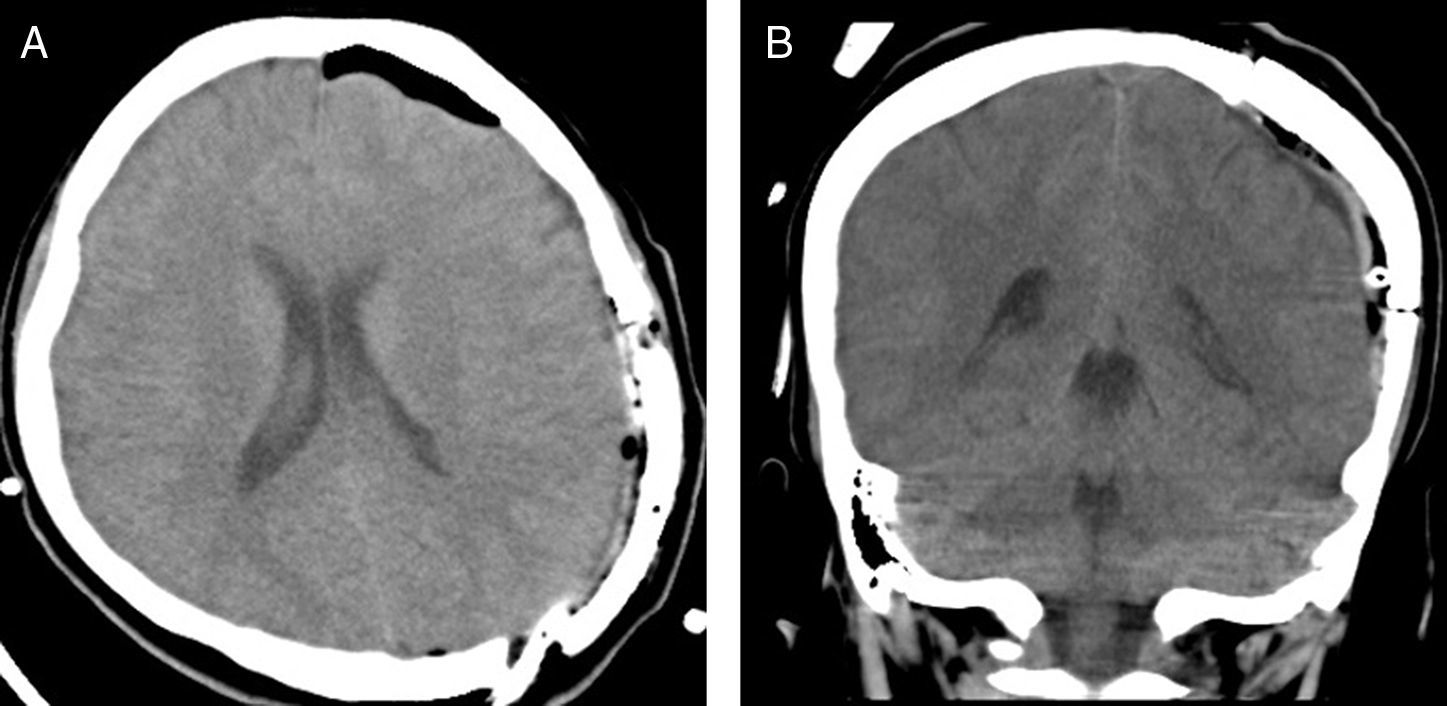
A 19-year-old female with sickle cell anemia (SCD) was referred to our hospital after two days of hospitalization at another hospital for a headache crisis. This headache crisis was due to a raised intracranial pressure; these symptoms were noted and included in her comprehensive list of symptoms. There was an acute drop in the hemoglobin and hematocrit levels. The cranial CT scan demonstrated a left fronto-parietal acute epidural hematoma (AEH) and a calvarial bone expansion, which was suggestive of medullary hematopoiesis. The patient underwent emergent craniotomy and evacuation of the hematoma. There were no abnormal findings intra-operatively apart from the AEH, except skull thickening and active petechial bleeding from the dural arteries. Repeated CT scan showed a complete evacuation of the hematoma. The possible underlying pathophysiological mechanisms were discussed. In addition to the factors mentioned in the relevant literature, any active petechial bleeding from the dural arteries on the separated surface of the dura from the skull could have contributed to the expanding of the AEH in our patient. Neurosurgeons and other health care providers should be aware of spontaneous AEH in patients with SCD.
Una mujer de 19 años con anemia de células falciformes (anemia drepanocítica) fue remitida a nuestro hospital tras 2 días de hospitalización en otro centro, debido a una crisis de migraña. Dicha crisis de migraña fue debida a un incremento de la presión intracraneal; se anotaron dichos síntomas y se incluyeron en su amplia lista de síntomas. Se produjo un pico agudo en los niveles de hemoglobina y de hematocrito. El escáner craneal mostró un hematoma epidural agudo fronto-parietal izquierdo y una expansión del hueso de la bóveda craneal, que indicaba una hematopoyesis medular. Se sometió a la paciente a una craneotomía de urgencia y a una evacuación del hematoma. Aparte de la anemia de células falciformes, los hallazgos intraoperatorios fueron: adelgazamiento craneal y petequia activa de las arterias durales. La repetición del escáner mostró la evacuación total del hematoma. Se analizaron los posibles mecanismos patofisiológicos subyacentes. Además de los factores mencionados en la literatura relevante, cualquier sangrado petequial activo de las arterias durales sobre la superficie separada de la duramadre, desde el cráneo, podría haber contribuido a la expansión del hematoma epidural agudo en nuestra paciente. Los neurocirujanos y demás facultativos sanitarios deberían tener conocimiento del hematoma epidural agudo espontáneo en pacientes con anemia de células falciformes.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.