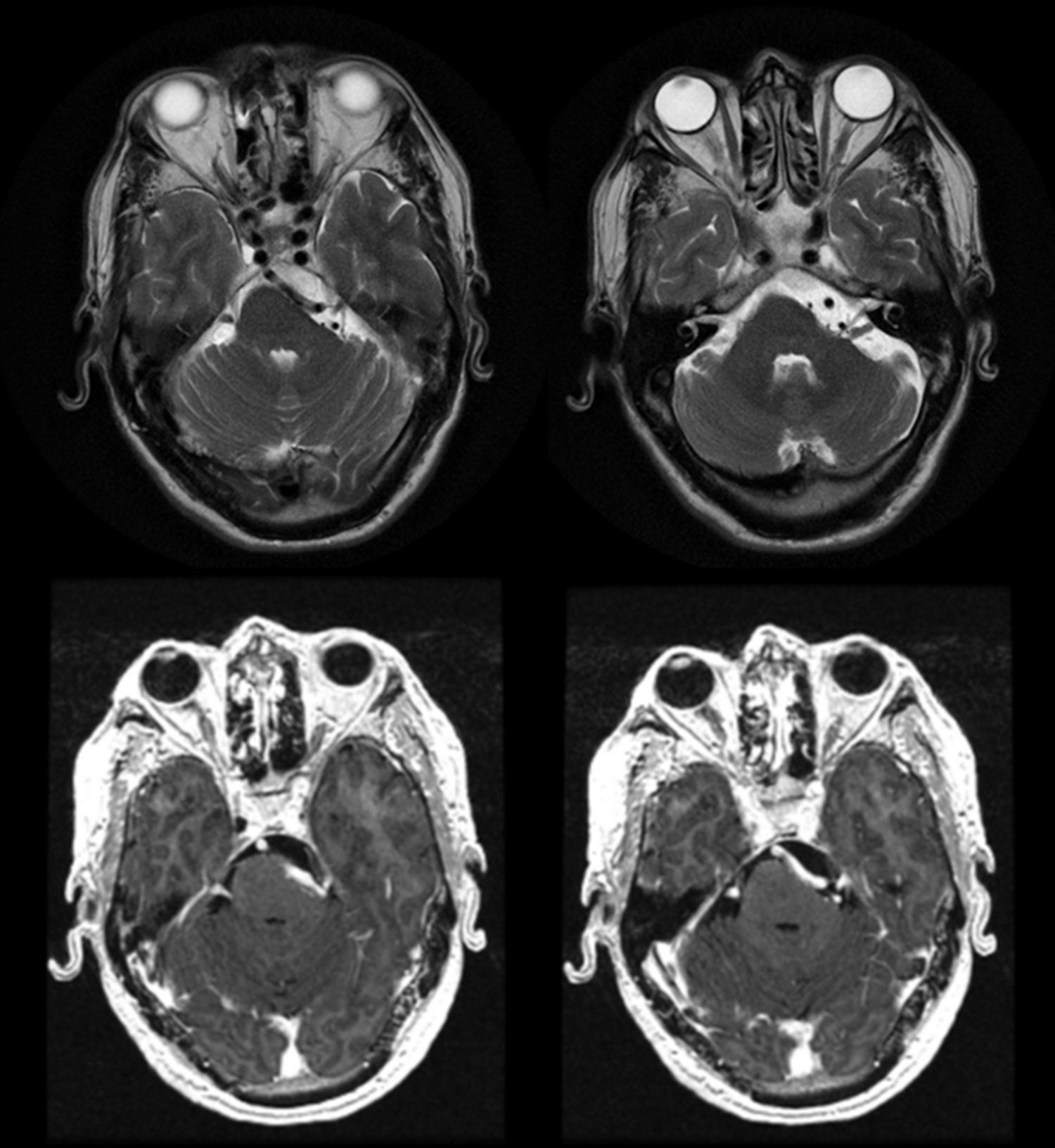
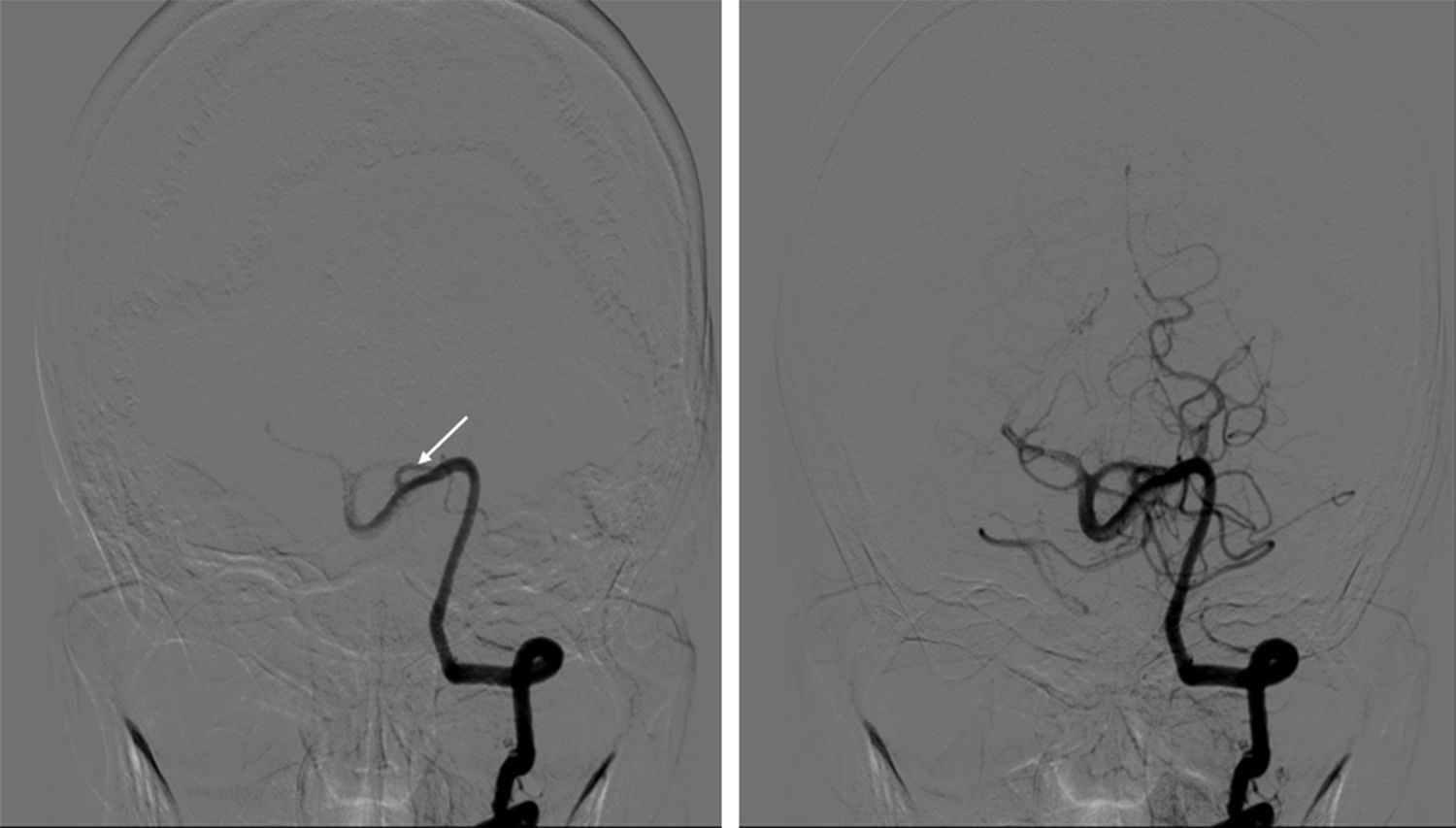
Vertebrobasilar dolichoectasia is a condition in which there is elongation and dilatation of the vertebral and basilar arteries. Few studies have been reported that focus on cases of trigeminal neuralgia (TN) secondary to vertebrobasilar dolichoectasia (VD) and treated by microvascular decompression (MD).
Patients and methodsA case is presented of trigeminal neuralgia caused by vertebral artery compression. An analysis of the microsurgical technique, as well as a systematic review of the literature about this uncommon nerve compression is performed, in order to investigate, by pooled case analysis, if MD is a good option for this type of patient.
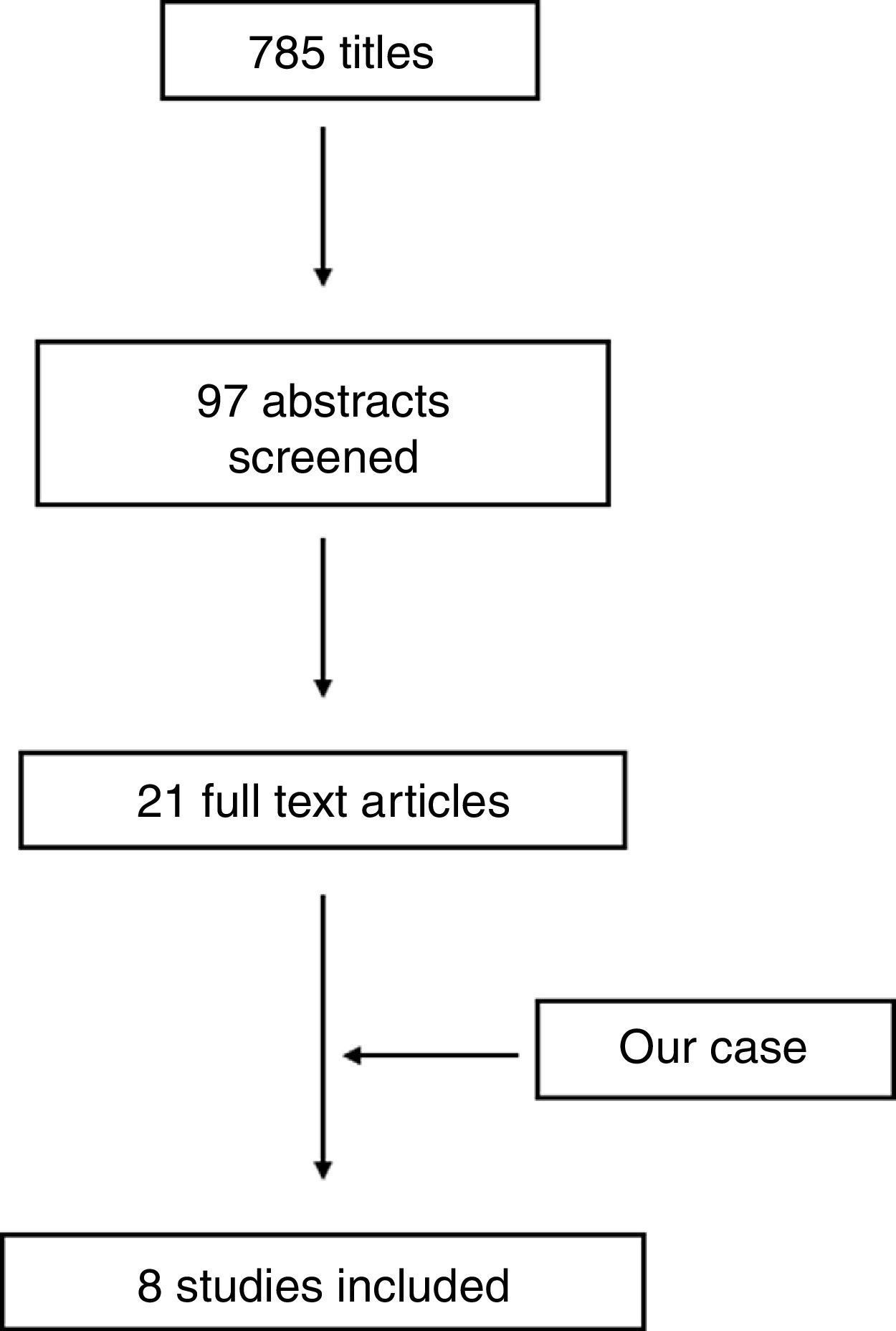
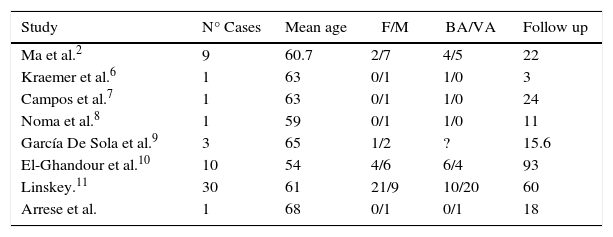
ResultsA total of 7 studies were included for analysis, to which the present case was added, making a total of 56 patents. There were excellent results in 53 cases, and partial recovery in 3, with a mean follow up of 54 months. No major complications were found.
DiscussionThe good clinical results and absence of postoperative mortality or severe morbidity in our pooled case series lead us to recommend MD as the preferred treatment for TN caused by VD in patients in whom major surgery is not contraindicated.
La dolicoectasia vertebrobasilar se caracteriza por la elongación y dilatación de las arterias vertebral y basilar. Muy pocos estudios se han enfocado a casos de neuralgia del trigémino secundaria a dolicoectasia vertebrobasilar tratada mediante descompresión microvascular.
Pacientes y métodosPresentamos un caso de neuralgia del trigémino causada por compresión de la arteria vertebral. Se realiza un análisis de la técnica quirúrgica así como una revisión sistemática de la literatura sobre este tipo de compresión poco común, con el fin de hacer un análisis de los casos para evaluar si la descompresión microvascular es una buena opción terapéutica.
ResultadosSeleccionamos 7 estudios que fueron incluidos en el análisis a los que añadimos nuestro caso, contando con un total de 56 pacientes. Se obtuvieron excelentes resultados en 53 casos y mejoría parcial en 3 con una media de seguimiento de 54 meses. No se encontraron complicaciones severas.
DiscusiónLos buenos resultados clínicos y la ausencia de morbimortalidad severa postoperatoria encontrados en nuestro estudio nos conducen a recomendar la descompresión microvascular como tratamiento de elección para pacientes con neuralgia del trigémino secundaria a compresión por dolicoectasia vertebrobasilar en pacientes en los que la cirugía mayor no esté contraindicada.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.