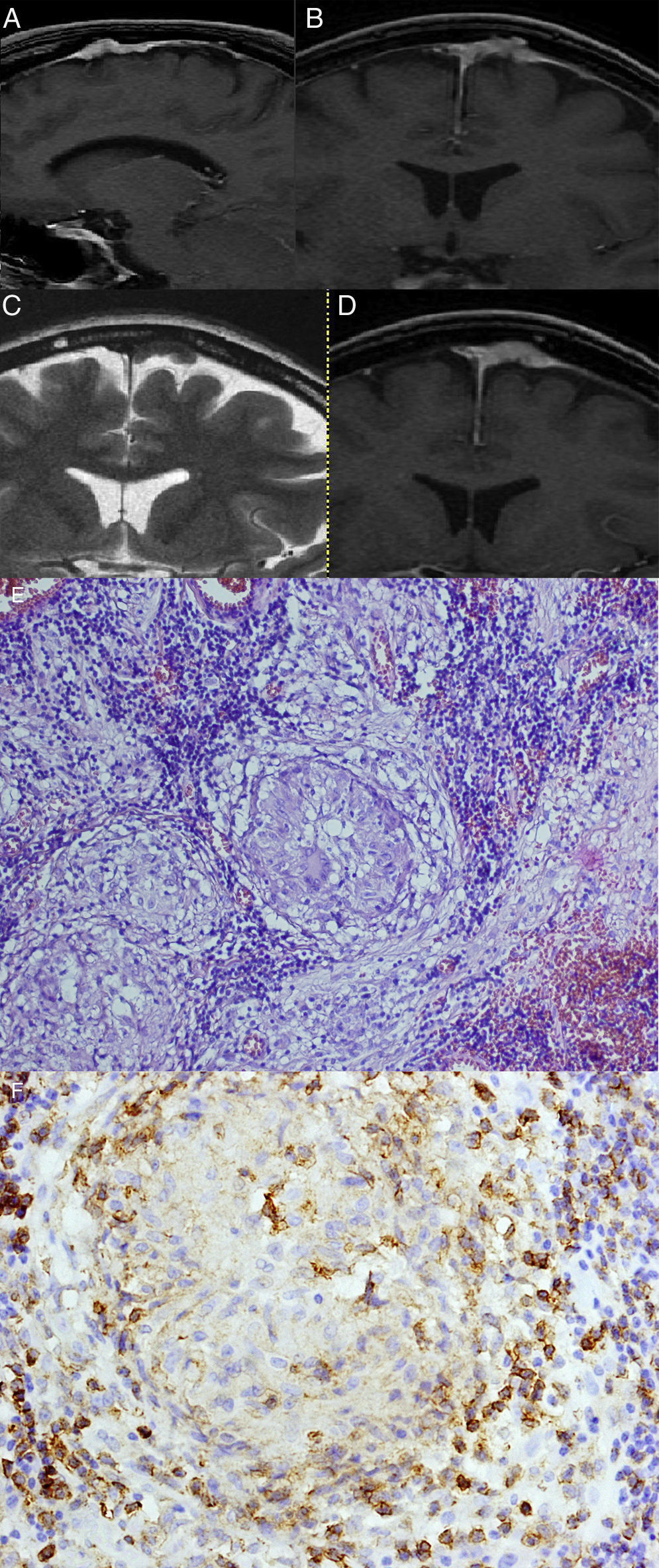
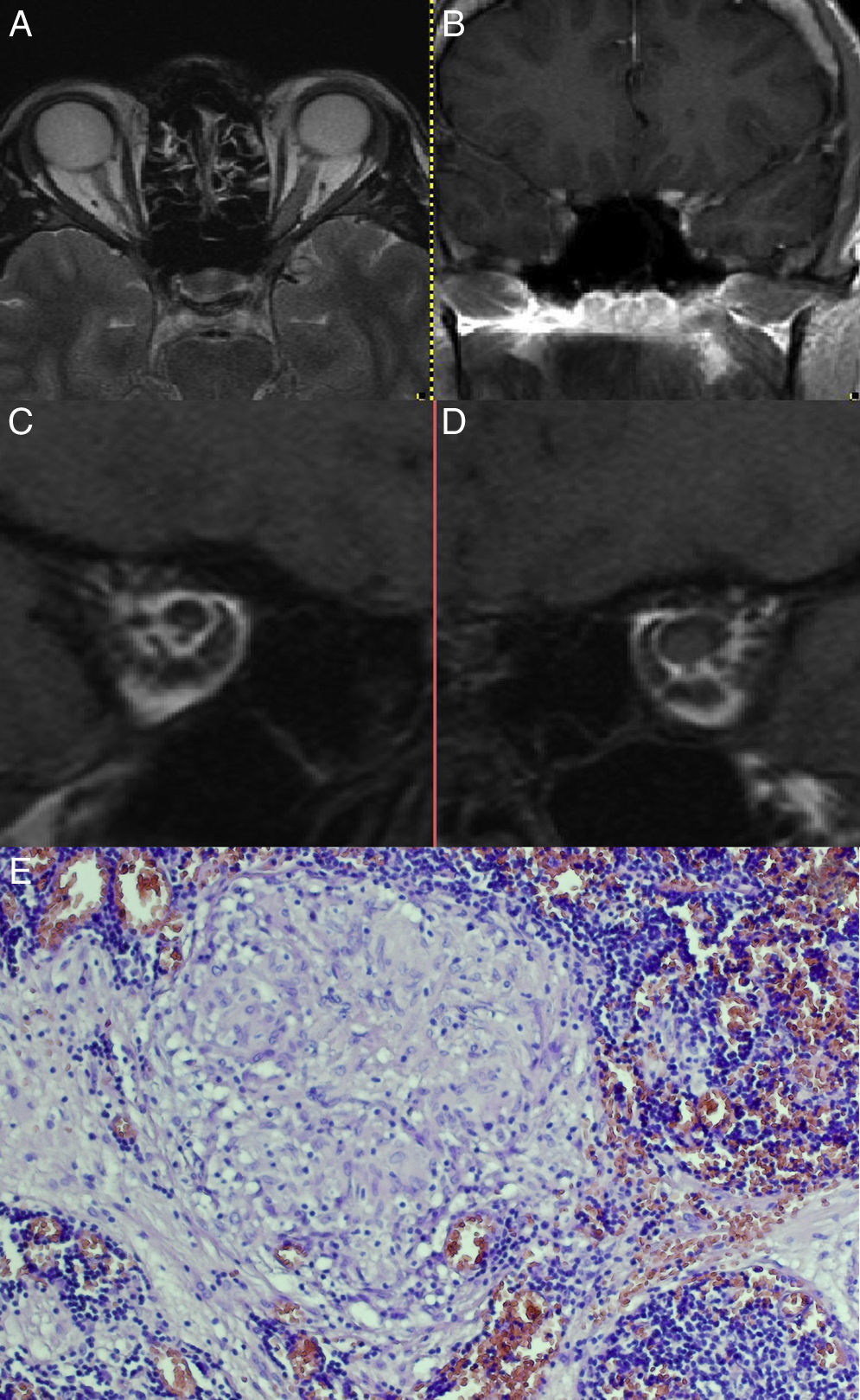
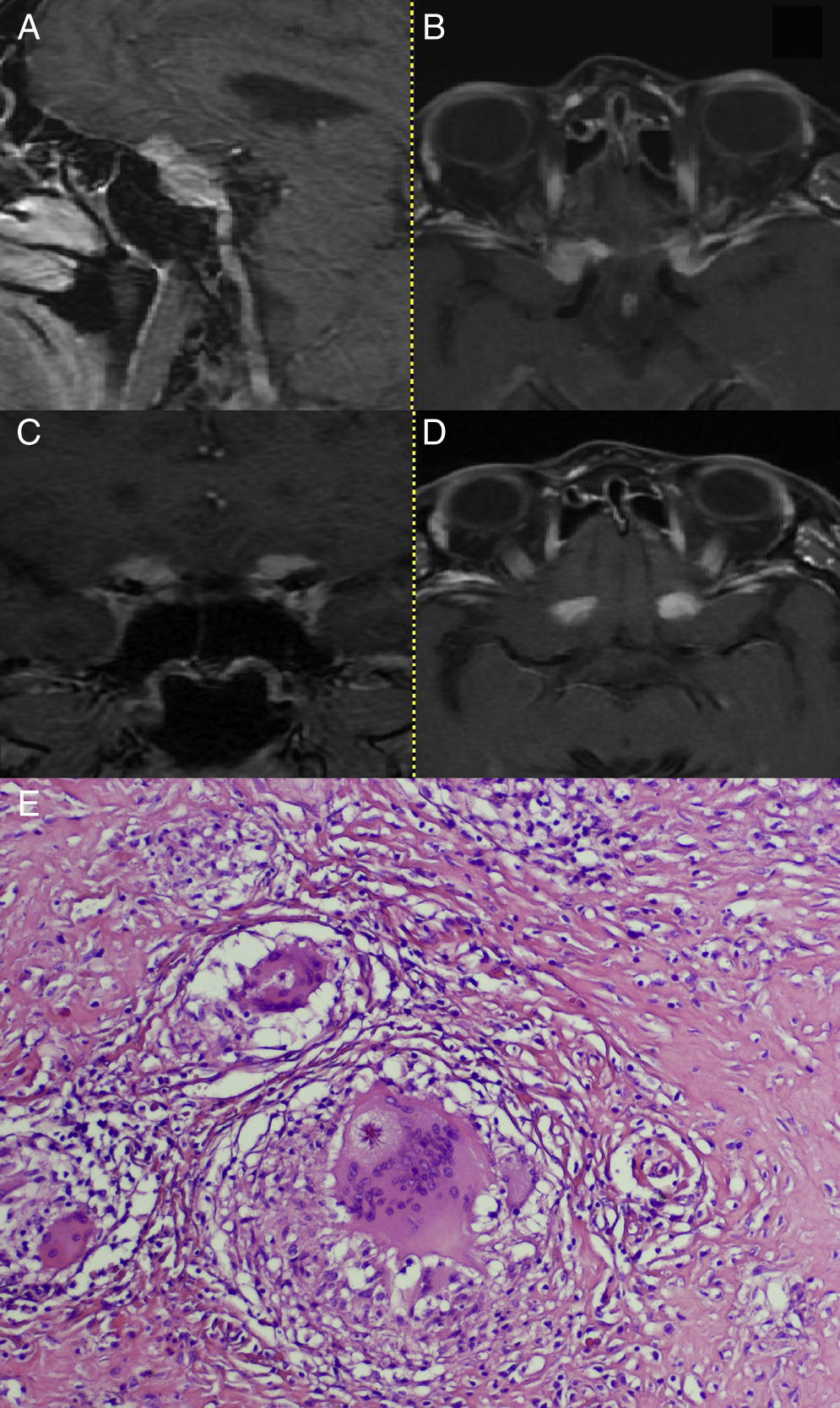
Isolated neurosarcoidosis (INS), as a disease of low prevalence, is commonly overlooked in differential diagnosis, and its discovery on histopathological examination usually comes as a surprise. Preoperative diagnosis is difficult because the clinical picture of INS is non-specific. Its symptoms depend on the location of the lesions, and the MRI results are similar to those found in meningiomas or optic nerve gliomas. Although up to 5% of all sarcoidosis patients present with neurological symptoms, those with INS are exceptionally infrequently encountered.
Three cases of INS are presented here, analysing their clinical course and radiological images, in order to determine characteristic traits that might lead to a correct diagnosis.
La neurosarcoidosis aislada (Isolated neurosarcoidosis - INS), como enfermedad de prevalencia baja, a menudo no es tomada en consideración en el diagnóstico diferencial, entonces su descubrimiento en los estudios histológicos generalmente llega inesperadamente. El diagnóstico preoperatorio es difícil porque el cuadro clínico de la INS no es específico pues sus síntomas dependen sólo de la localización de las lesiones, mientras que los resultados de RM son parecidos a los encontrados en los meningiomas o gliomas del nervio óptico. Aunque hasta el 5% de todos los pacientes con sarcoidosis presentan síntomas neurológicos, aquellos con INS se encuentran excepcionalmente.
Presentamos tres casos de INS, analizando su curso clínico y la imagen radiológica para determinar unos síntomas típicos que podrían ayudar a realizar el diagnóstico correcto.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.