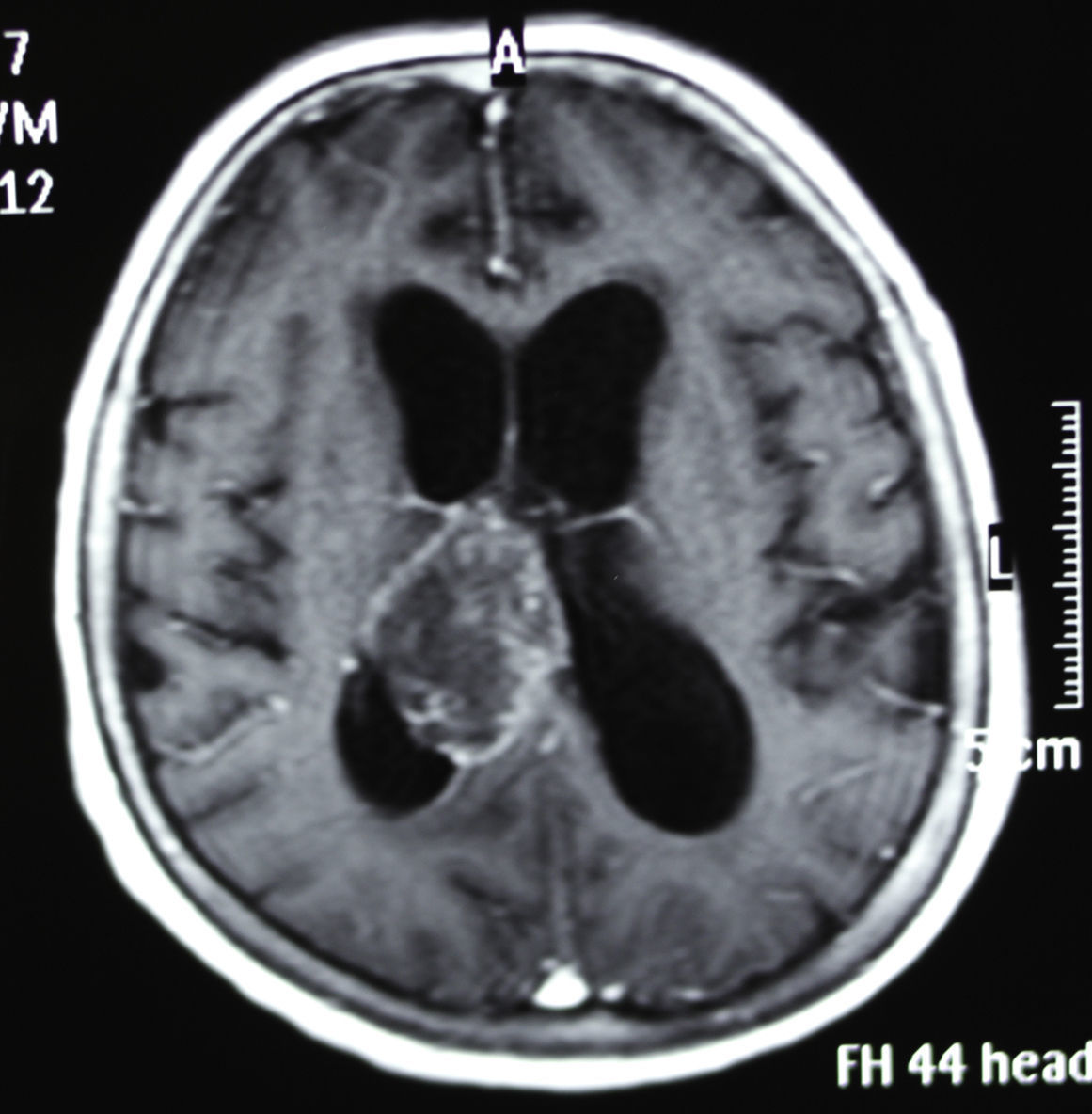
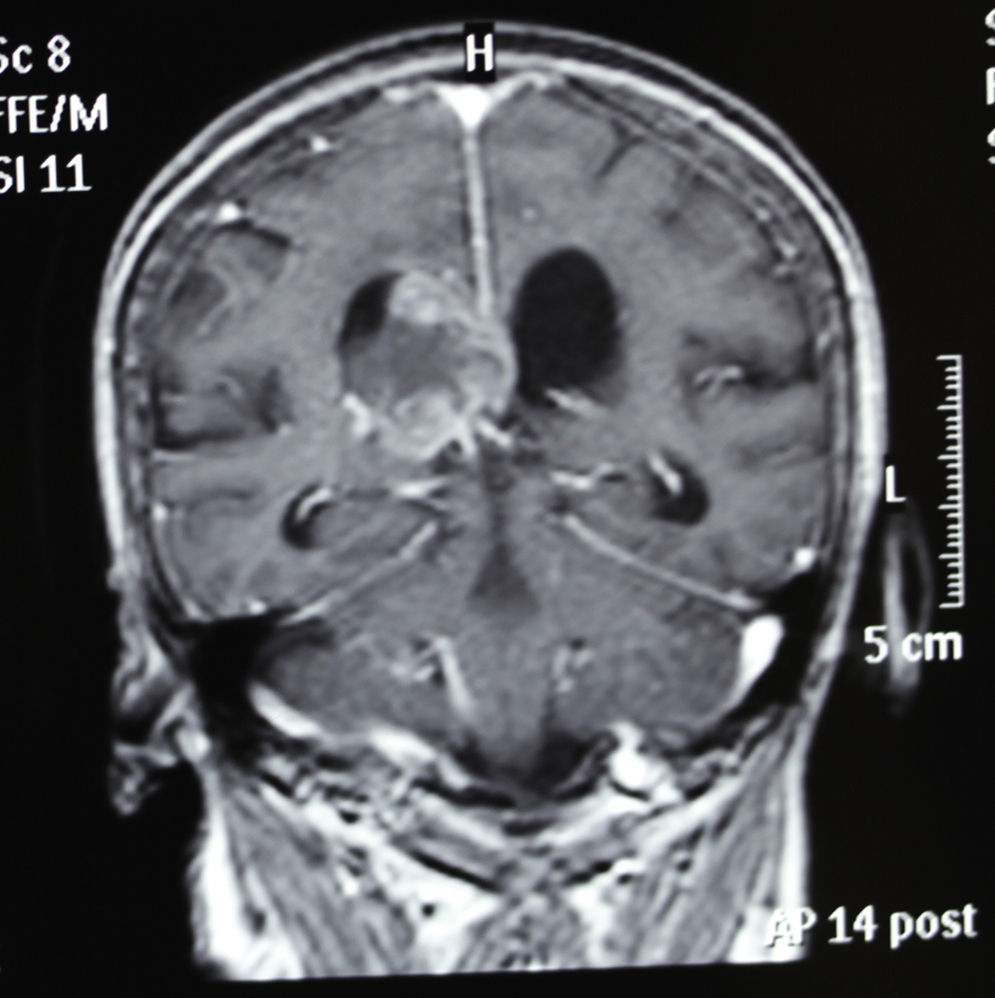
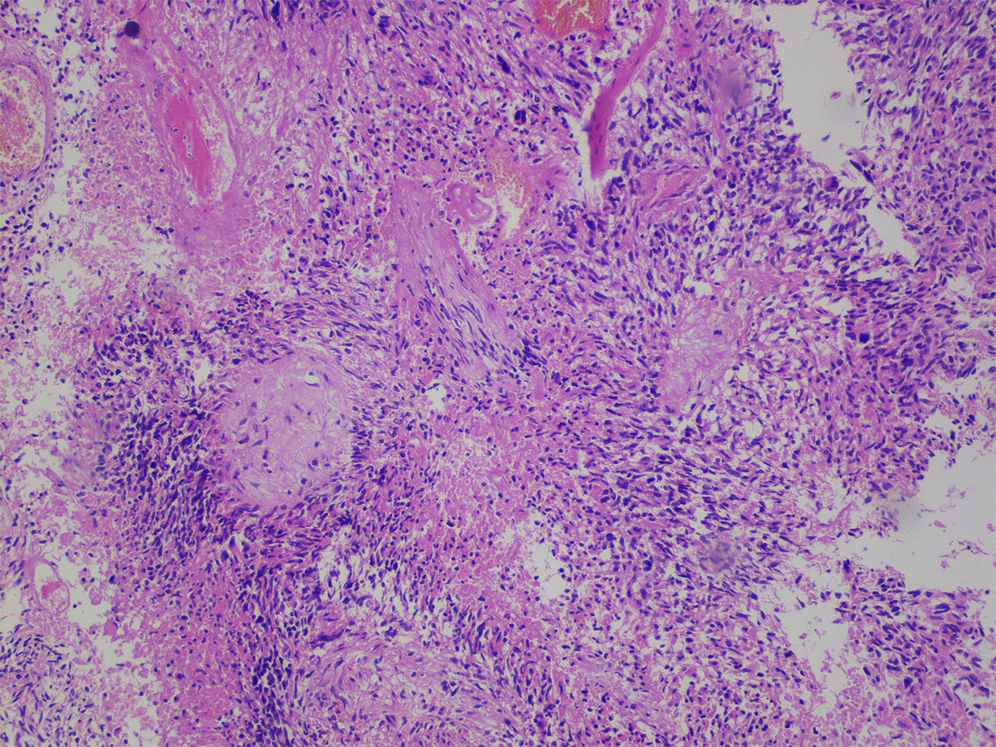
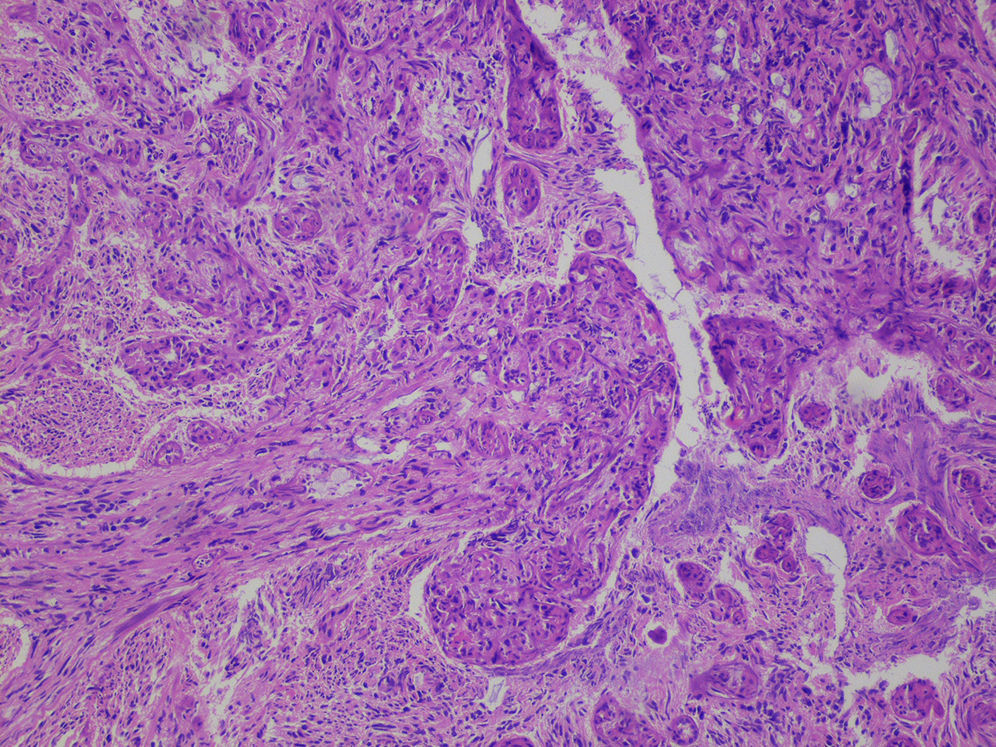
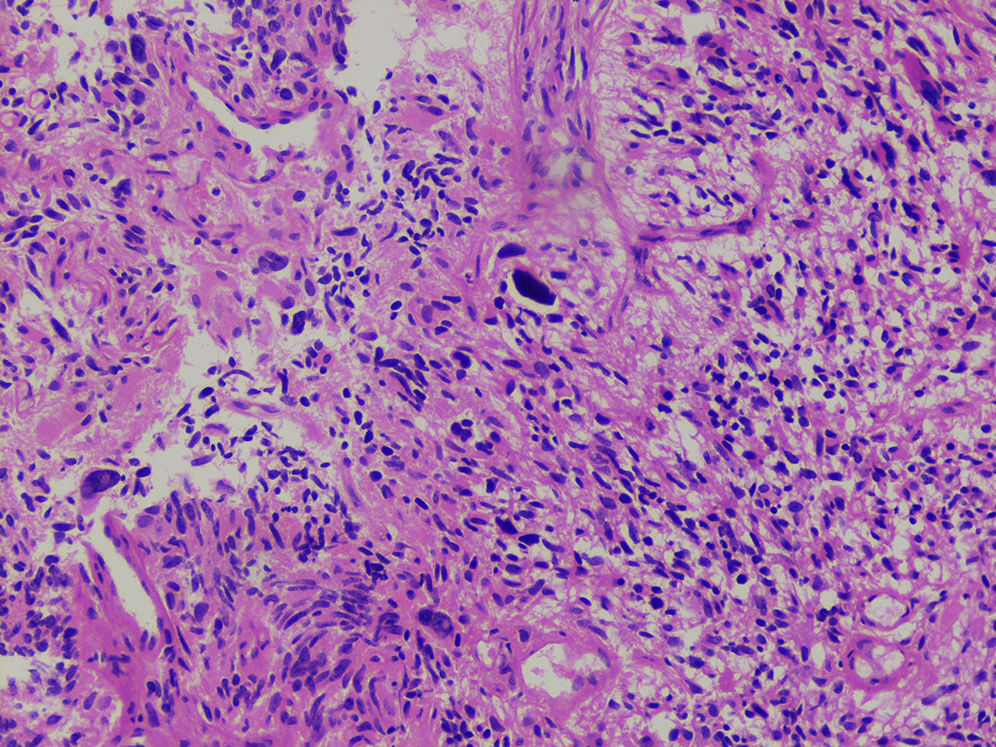
Glioblastoma multiforme (GBM) is the most common primary brain tumor, but pure intraventricular location is extremely rare for GBM in neurosurgical practice. To our knowledge, there are only 19 reported cases to date. We present an additional case of intraventricular GBM with detailed clinical course, radiological and pathological findings.
El glioblastoma multiforme (GBM) es el tumor cerebral primario más común que existe, pero una localización netamente intraventricular es muy rara en la práctica neuroquirúrgica. Según nuestro conocimiento, hasta la fecha solo se han publicado 19 casos intraventriculares. Presentamos un nuevo caso de GBM intraventricular con una descripción detallada de la evolución clínica y los hallazgos patológicos y radiológicos.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.