Deep Brain Stimulation (DBS) is a therapeutic option for some forms of Parkinson's disease (PD). The main adverse effects of this surgery are: infection (2–9%), haemorrhage (1–4%) and seizures (1–3%). We report a rare complication of DBS: an intracranial abscess.
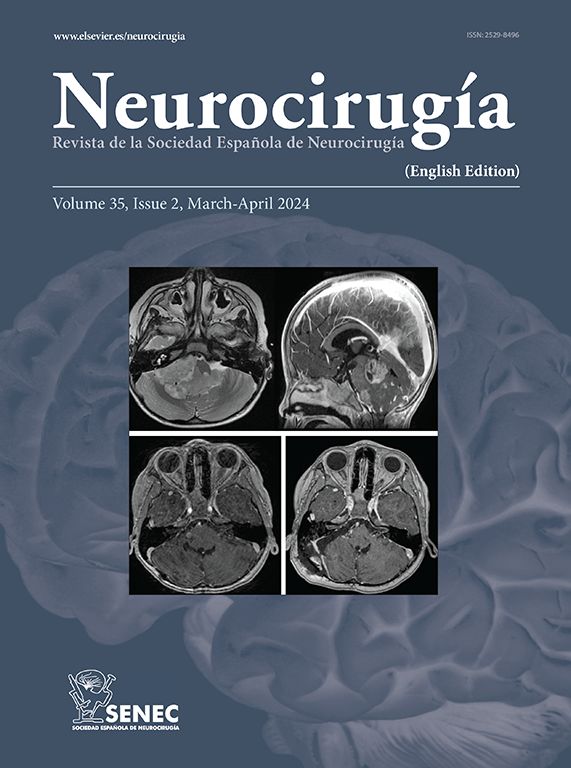
Case reportA 59-year-old male who had suffered PD for 19 years was submitted to bilateral subthalamic nucleus DBS in September 2003, when he was 52. One month later, he developed an inflammatory reaction of the skin and subcutaneous tissue surrounding the area of the subcutaneous DBS system. No infectious agent was isolated. In the following 12 months he required 5 major surgeries due to a process of systematic inflammation/infection throughout different locations of the DBS system. A few days after removal of the DBS device, he developed a right oculomotor nerve paresis and mild left hemiparesis. A CT scan revealed an abscess in the right thalamo-mesencephalic area. Both the new neurological deficits and the previous tremor and rigidity improved after surgical drainage and medical treatment.
ConclusionThis case report illustrates a rare complication of DBS surgery. Nevertheless, Parkinsonism improved, probably because the abscess acted like a subthalomotomy.
La estimulación cerebral profunda (DBS) es una opción terapéutica en algunas formas de la enfermedad de Parkinson (PD). Sus complicaciones principales son las infecciónes (2–9%), las hemorragias (1–4%) y las convulsiones (1–3%). Se presenta una complicación rara de la DBS: un absceso intracraneal.
Caso clínicoUn paciente de 59 años fue enviado para estimulación bilateral del núcleo subtalámico en setiembre del 2003 tras 19 años de enfermedad. Un mes más tarde desarrolló una reacción inflamatoria de la piel y tejido subcutáneo en las zonas adyacentes al sistema de DBS, no se consiguiendo aislar ningún microorganismo. Durante los 12 meses siguientes fueron necesarios cinco drenajes quirúrgicas por infecciones o inflamaciones en diferentes localizaciones del sistema. Finalmente se decidió retirar todo el sistema, pero unos días más tarde desarrolló una paresia del III par derecho y una discreta hemiparesia izquierda. Un TAC cerebral reveló la presencia de un absceso en la región talamo-mesencefalica. Tanto estos últimos déficits, como el temblor y la rigidez previos, mejoraron después del drenaje quirúrgico y del tratamiento médico.
ConclusiónEste caso, ilustra una complicación rara de la cirugía de DBS. Sin embargo el paciente mejoró de su Parkinson ya que el absceso se “comportó” como una subtalamotomía.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.