Intracranial meningiomas without dural attachment (MWODA) are rare entities. We present the first case published, to the best of our knowledge, regarding a MWODA attached to the ventral surface of the brainstem. This location makes the patient subsidiary to treatment through an expanded endonasal transclival approach.
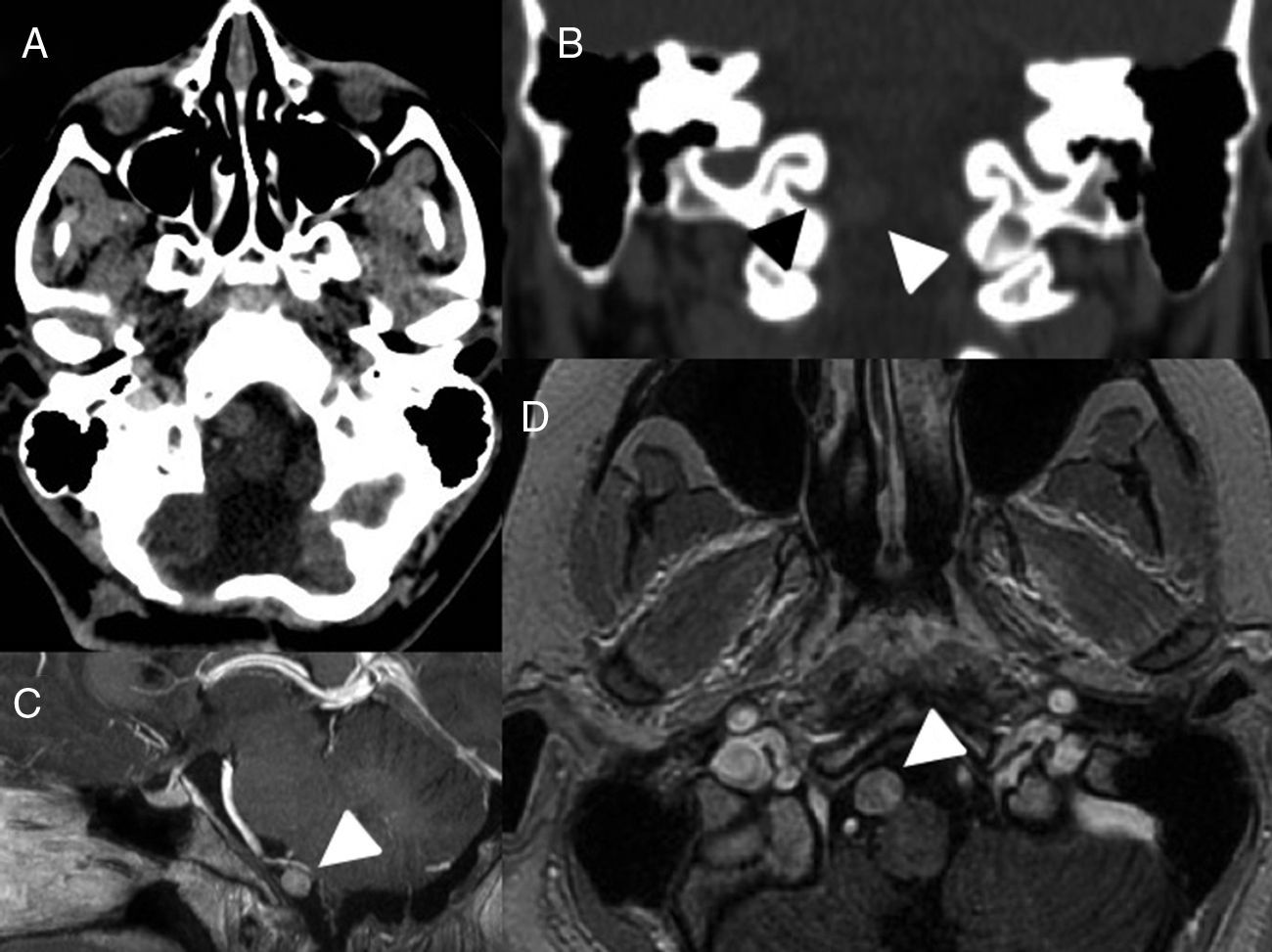
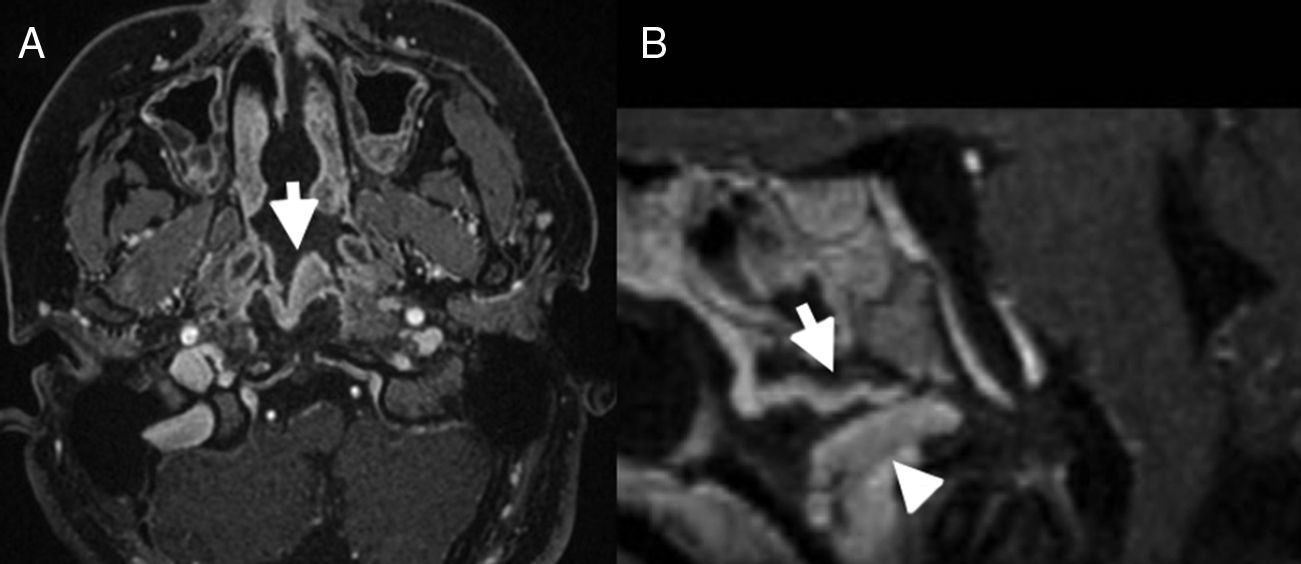
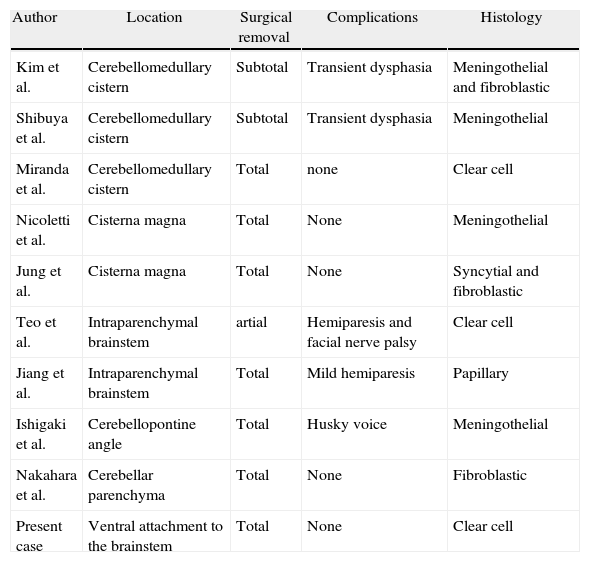
Clinical presentationA 16-year-old female with suspected diagnosis of recurrence of a clear cell meningioma (CCM) at a distance from the initial lesion, located on the premedullary cistern. The patient underwent a pure endoscopic low transclival approach. The attachment to the ventral surface of the brainstem was confirmed intraoperatively. Postoperative MRI confirmed gross total resection and treatment was complemented with adjuvant fractionated stereotactic radiotherapy. No complications related to the procedure were observed.
ConclusionMWODA may appear attached to the ventral brainstem. The expanded endonasal approach to the clivus provides a critical anatomical advantage in the treatment of medial lesions, even ventral meningiomas, to the lower cranial nerves. Reconstruction principles must be strictly respected to reduce complications.
Los meningiomas sin implantación dural MSID son una rara entidad. Presentamos el primer caso publicado en nuestro conocimiento, de MSID implantado en la superficie ventral del tronco cerebral. Dicha localización permite la realización de un abordaje quirúrgico endonasal expandido transclival para su tratamiento.
Caso clínicoPaciente mujer de 16 años con la sospecha de presentar una recurrencia de meningioma de células claras localizada en la cisterna prebulbar a distancia de la lesión inicialmente tratada. Se llevó a cabo un abordaje endonasal expandido transclival. El hallazgo de implantación en la cara ventral del tronco cerebral fue claramente evidenciado en el acto quirúrgico. La RM cerebral postoperatoria confirmó la resección completa y el tratamiento fue completado con radioterapia estereotáctica fraccionada. No se presentaron complicaciones relacionadas con los procedimientos.
ConclusiónLos MSID pueden presentarse en íntima relación con la cara ventral del tronco cerebral. El abordaje endonasal expandido transclival otorga ventajas anatómicas importantes a la hora de tratar lesiones de localización medial, incluso meningiomas ventrales a los pares craneales bajos. Las técnicas reconstructivas deben ser estrictamente respetadas para minimizar complicaciones.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.