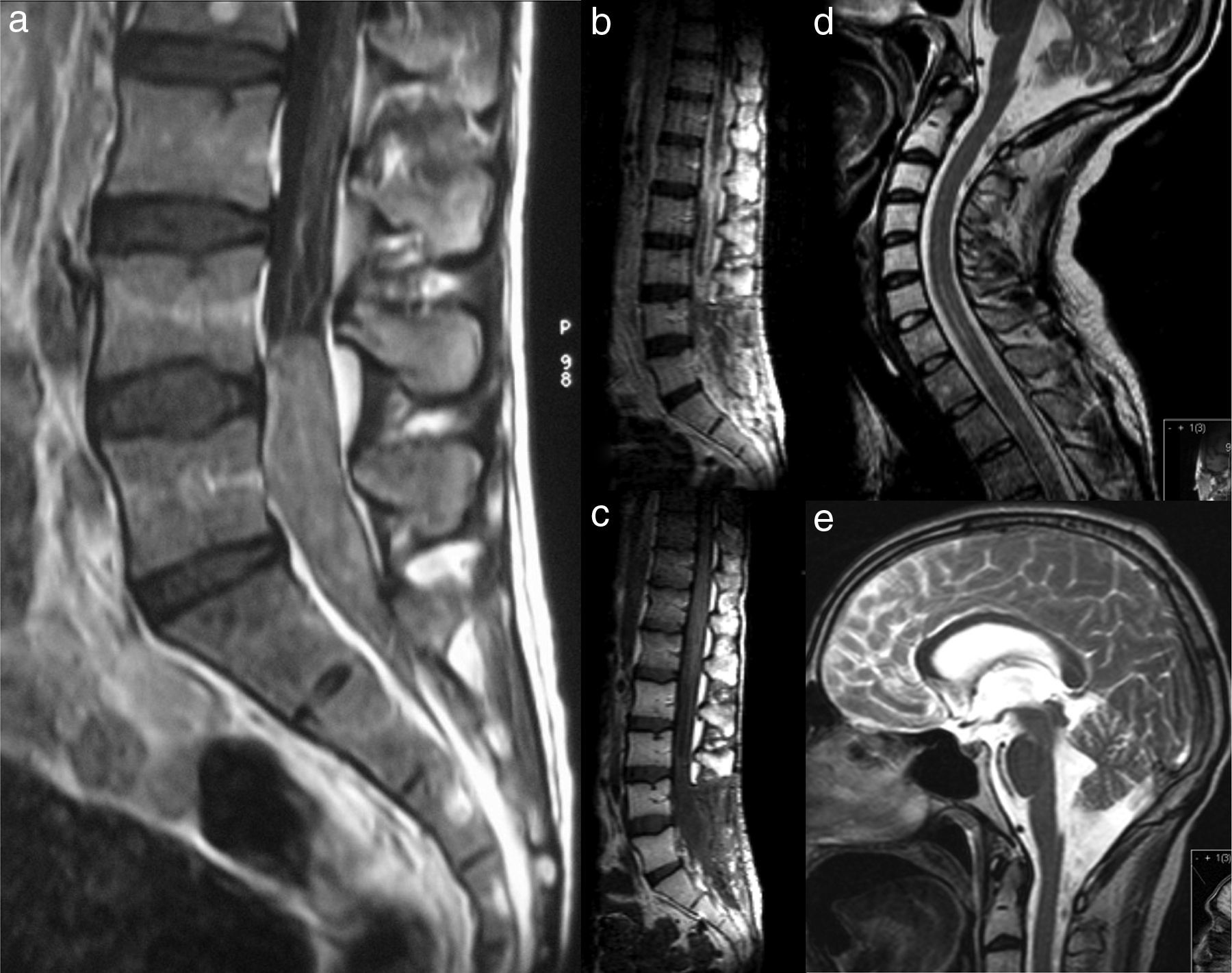
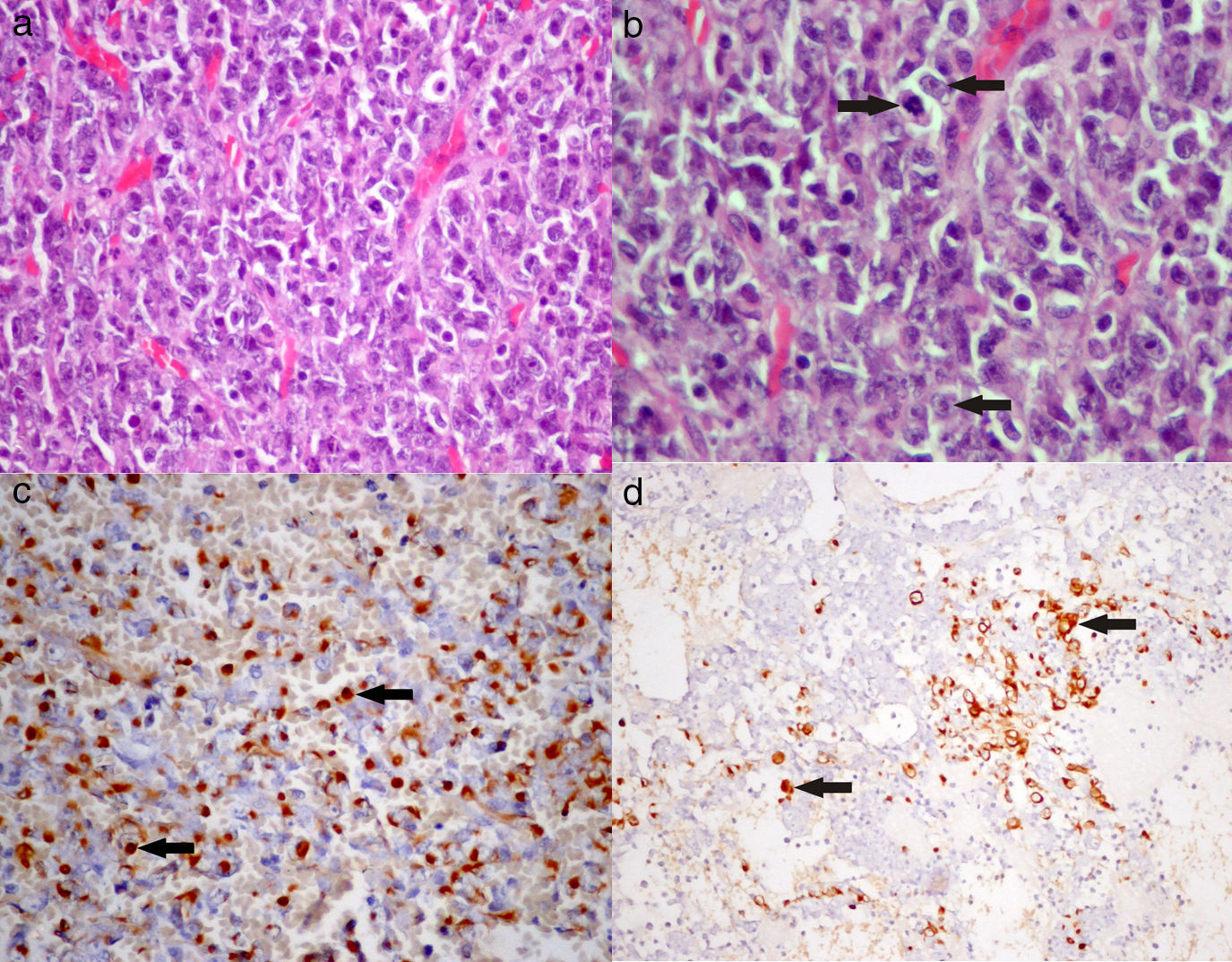
Epithelioid sarcomas are rare mesenchymal neoplasms mainly arising in the limbs of young adults. We report the case of a 24-year-old male presenting low back pain radiating to both lower limbs, constipation and urinary retention. The MRI scan showed an intraspinal lesion extending from L4 to S2. Surgery resulted in gross total removal of the extradural lesion and partial removal of the intradural component. The immunohistological study of the lesion was consistent with an epithelioid sarcoma. The patient was submitted to radiotherapy and chemotherapy, but a local recurrence of the lesion and dissemination along the neuraxis were observed 3 months after surgery. Despite treatment, the patient died 4 months after the surgical procedure due to multiorgan failure.
Despite there being isolated reports of epithelioid sarcomas appearing in the spine, this is, to our knowledge, the first case with intradural extension.
Los sarcomas epitelioides son neoplasias mesenquimatosas raras que afectan sobre todo a extremidades de adultos jóvenes. Presentamos el caso de un adulto de 24 años de edad y sexo masculino que consulta por lumbalgia irradiada a miembros inferiores, estreñimiento y retención urinaria. La RM mostró una lesión espinal que se extendía de L4 a S2. La cirugía consistió en una resección casi total de la lesión extradural y parcial del componente intradural.
El estudio inmunohistológico de la lesión fue compatible con un sarcoma epitelioide. El paciente fue sometido a radioterapia y quimioterapia, pero 3 meses después de la cirugía se verificó recurrencia local de la lesión y diseminación tumoral a lo largo del neuroeje. A pesar del tratamiento, el paciente falleció 4 meses después de la cirugía por fallo multiorgánico.
Este es el primer caso descrito en la literatura de sarcoma epitelioide espinal con extensión intradural.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.