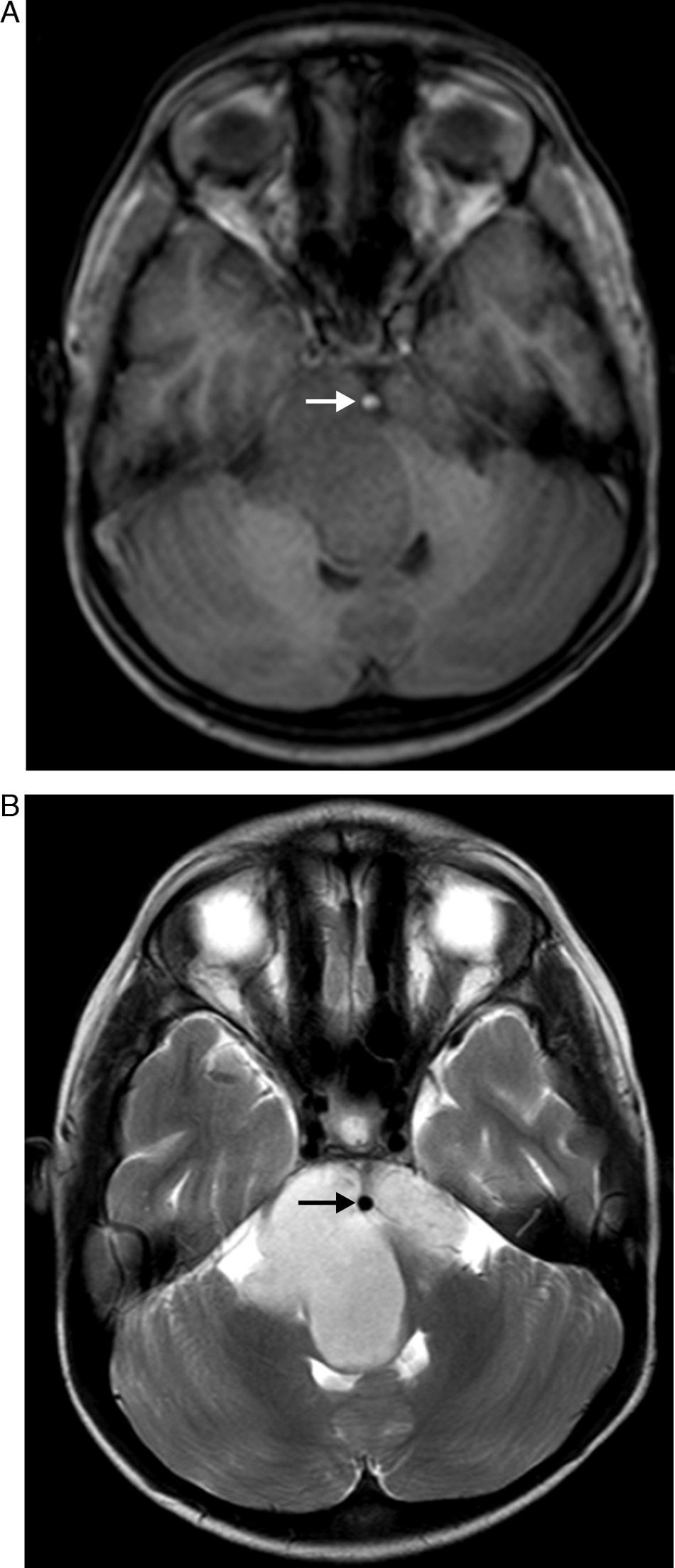
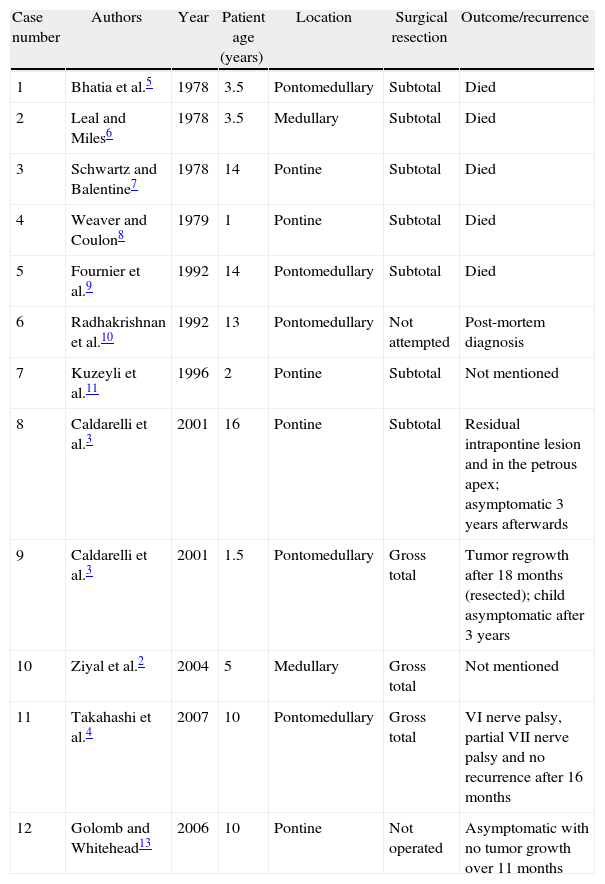
To describe an atypical clinical and radiological presentation of a brainstem epidermoid cyst in a child and to provide a review of the medical literature on brainstem epidermoid cysts in children.
Material and methodReview of medical records and operative notes of an unusual case of a patient with a brainstem epidermoid cyst. MEDLINE literature search using the terms brainstem, epidermoid cyst and children.
ResultsGross total resection of the cyst was achieved. The patient had an uneventful recovery.
ConclusionEpidermoid cysts are rare tumors of the brain and children. The management of these tumors can be quite challenging. A good clinical and neuroradiological evaluation pre-operatively is fundamental for a successful surgical treatment. Surgical resection should be as radical as possible without putting the patient's neurological status into risk.
Describir una presentación atípica clínica y radiológica de un quiste epidermoide del tronco cerebral en un niño y hacer una revisión de la literatura médica sobre los quistes epidermoides del tronco cerebral en los niños.
Material y métodoRevisión de historias clínicas y notas operativas de un caso inusual de un paciente con un quiste epidermoide del tronco cerebral. Búsqueda bibliográfica de los términos tronco encéfalico, quiste epidermoide y niños.
ResultadosLa resección quirúrgica completa del quiste se logró. El paciente tuvo una recuperación sin complicaciones.
ConclusiónLos quistes epidermoides son tumores poco frecuentes en el cerebro y su manejo implica algunos riesgos. Una buena evaluación clínica y radiológica antes de la operación es fundamental para un tratamiento quirúrgico exitoso. La resección quirúrgica debe ser tan radical como sea posible sin poner el estado neurológico del paciente en riesgo.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.