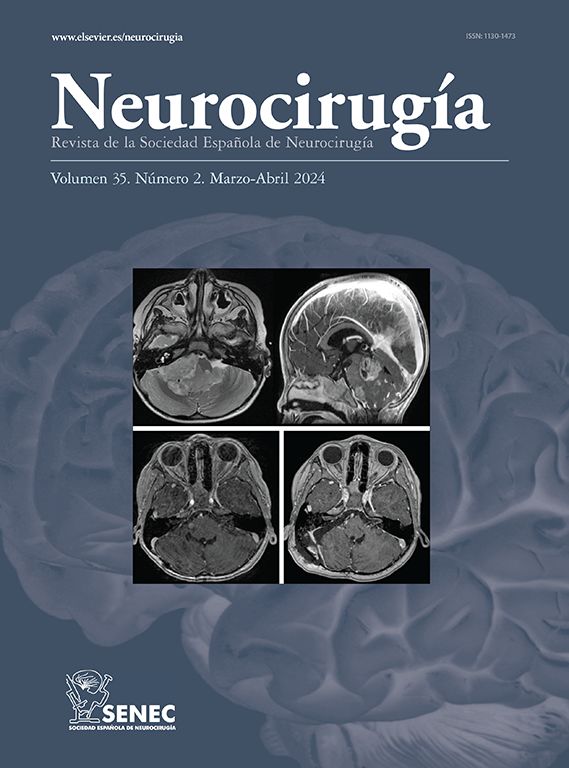
Brainstem Cavernomas
Neurosurgery, Cerebrovascular/Endovascular/Skull Bases Neurosurgery, University Hospital Cleveland Medical Center, Case Western Reserve University, Cleveland, Ohio, USA.
The understanding of brainstem cavernomas (CM) continues to evolve with studies of natural history epidemiology and operative and non-operative management. These lesions in the brainstem behaves differently than their supratentorial counterparts. Large series have shown an increase hemorrhage rate with a prior rupture during observational period compared to initial hemorrhage rate. Several studies found an annual bleed risk at 0.6% without a prior rupture, which is similar to their supratentorial lesions. With a history of prior bleed, the increased annual risk ranges from 3.1% to 6.5% in a number of studies.
Patient selection is key to optimal management. Patients with accessible lesions that are either exophytic, with repeated hemorrhages, or acute extralesional hemorrhages are potential surgical candidates. Advances in skull base surgery techniques and equipment as well as intraoperative image navigation have improved safer corridors for resection of brainstem CM with acceptable morbidity and mortality compared to repeated hemorrhages. Even deep seated brainstem CM without cortical hemosiderin staining can be safely resected, but only with accurate intraoperative image navigation.
The surgical approach to brainstem CM depends on its location. The 2-point method, where one point is placed at the center of the lesion and the other point is placed closest to the pial surface or the safest entry point dictates the specific approach. Essentially, one or combination of these five surgical approach can safely access any brainstem CM without having to perform more invasive approaches: 1) modified orbitozygomatic for interpendicular CM; 2) retrosigmoid for pontine CM; 3) Far lateral for anterior cervico-medullary CM; 4) suboccipital with and without telovelar for 4th ventricular CM; 5) lateral infratentorial supracerebellar for lateral midbrain and ponto-mesencephalic CM.