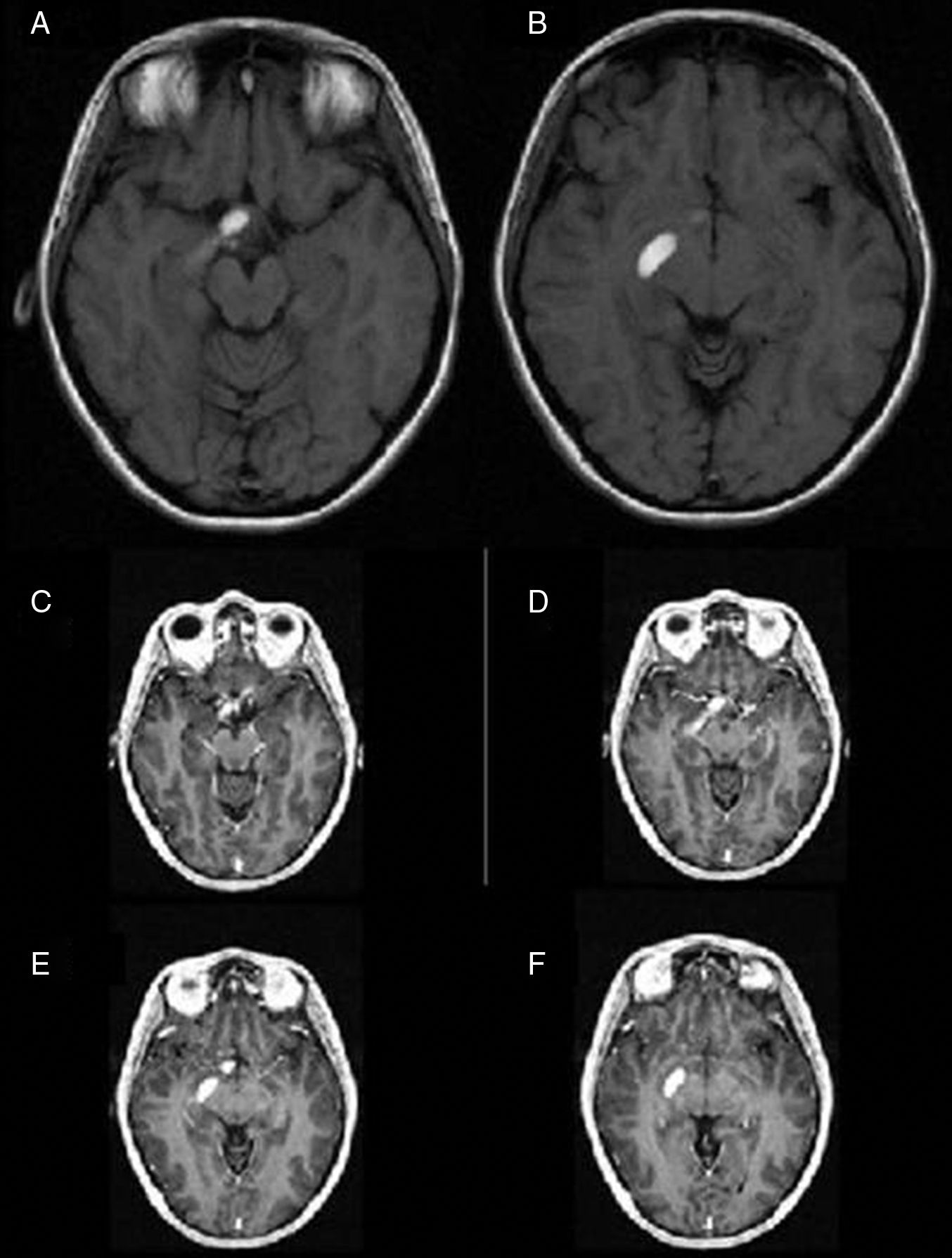
To report a unique case of haemorrhagic presentation of a chiasmal and optic tract glioma (OPG) appearing as an extra-axial lesion on MRI scans.
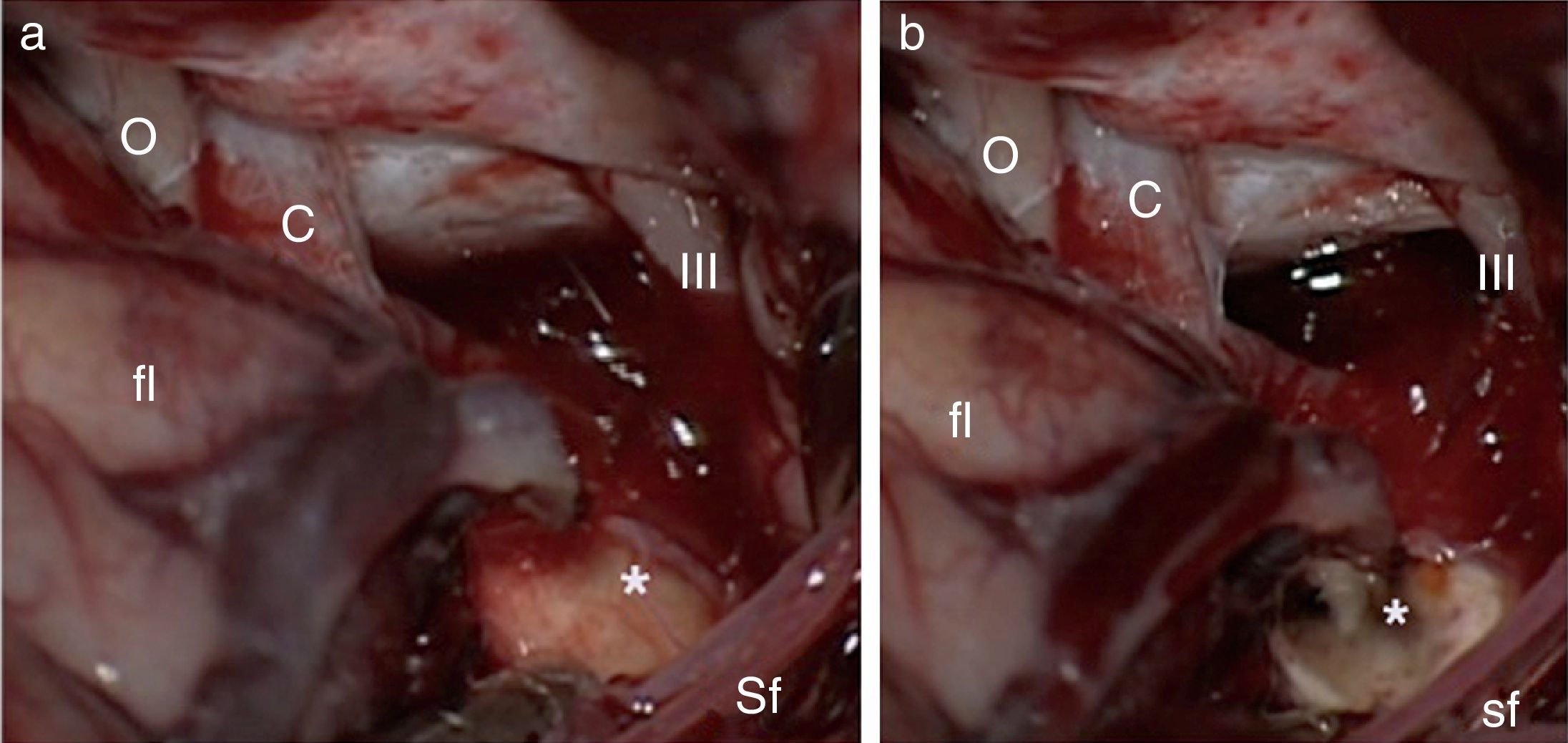
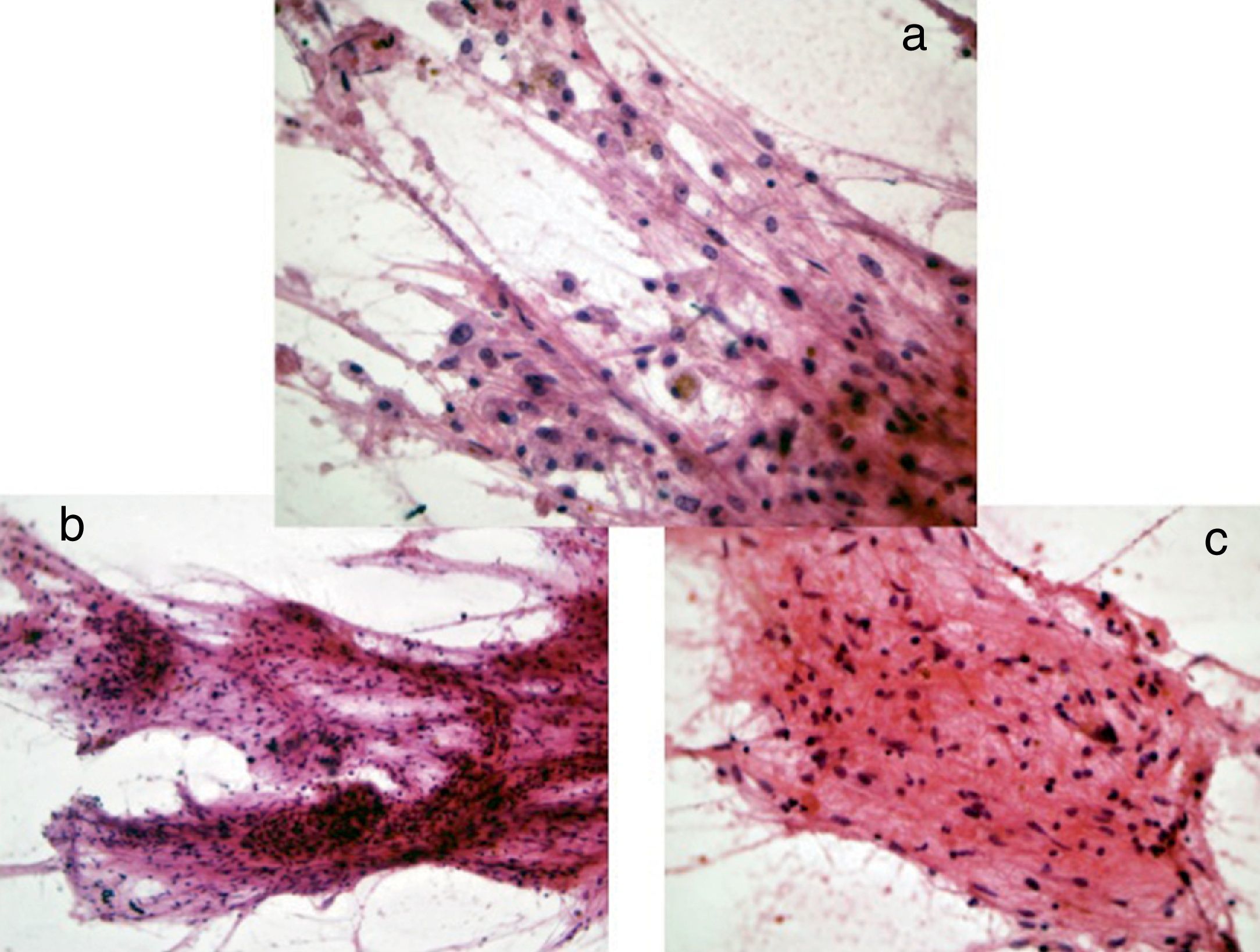
Case reportA 30-year-old female with a preoperative radiological diagnosis of dermoid cyst was operated. No lesion was found in the chiasmal or carotid cisterns within the operative field. The right posterolateral corner of the chiasma and the beginning of the right optic tract appeared swollen. The area was incised and a haemorrhagic fluid poured through the opening. Several samples were taken and the pathological diagnosis was of pilocytic glioma.
ConclusionsWe present a unique case of chiasmal bleeding into the optic pathway secondary to an optic glioma which radiologically mimicked an intracisternal cyst. In similar cases, rapid clinical evolution of the symptoms may be vital for the differential diagnosis. Surgery is warranted to prevent permanent damage to the visual pathway.
Reportamos un caso de presentación hemorrágica de un astrocitoma pilocítico quiasmático (APQ) que aparentaba una masa extraaxial en RM.
Caso clínicoMujer de 30 años que fue intervenida con diagnóstico preoperatorio de quiste dermoide pero que, en el campo quirúrgico, no se encontró lesión alguna en las cisternas quiasmática ni carotídea. A nivel del borde posterolateral del quiasma se apreciaba una zona enrojecida y abombada que, tras su incisión, demostró la presencia de hemorragia quiasmática. Las muestras tomadas en esta zona fueron diagnosticadas anatomopatológicamente de astrocitoma pilocítico.
ConclusionesPresentamos un caso excepcional de sangrado quiasmático de un APQ que imita radiológicamente una lesión extraaxial. En casos similares, la rápida evolución clínica puede ser la clave para el diagnóstico deferencial. La cirugía está justificada a fin de evitar daños visuales permanentes.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.